Experience in implementing a program for basic life support and available automated defibrillation in a cancer center
Аннотация
Unified approaches to ensuring the chain of survival can improve the patient’s prognosis both in out-of-hospital and in-hospital cardiac arrest.
Aim. To discuss practical issues of introducing a program for the availability of automated external defibrillation in a cancer center.
Material and methods. For four years, our healthcare facility has been implementing a training program for basic and advanced life support according to the European Resuscitation Council standards, combined with the creation and development of an infrastructure for the availability of automatic defibrillation. A roadmap and infrastructure were developed for the project implementation.
Results. In 2018-2022, 229 employees (114 doctors, 85 nurses and 30 nonmedical workers) were trained under the basic life support program. Fifteen defibrillators were placed in various units. During the specified period, first aid in case of sudden cardiac arrest using an automated external defibrillator before the resuscitation team arrival was independently provided by doctors and nurses of departments three times. To implement training in the continuous education system, the curriculum has passed the examination and accreditation in the edu. rosminzdrav system.
Conclusion. The development and implementation of such initiatives requires significant organizational and methodological work, including continuous education system. However, in our opinion, this is an extremely useful tool for improving the safety and quality of medical care.
Sudden cardiac arrest (SCA) is one the most common causes of death nowadays. Despite the significant progress in the prevention and treatment of heart and vascular diseases achieved in the last decade, mortality from sudden cardiac arrest remains high [1]. For example, in USA, almost 400 thousand cases of SCA occur every year at the prehospital stage, and only 12% of these patients survive [2][3]. The majority of out-of-hospital cardiac arrests (~80%) occur in houses and other residential premises [4][5]. The numerous studies showed that early defibrillation and availability of a trained lifeguard who is able to recognize cardiac arrest and to start resuscitation measures before the arrival of qualified help, can increase survival rate in case of both outof-hospital and intrahospital cardiac arrests [6-9]. One study evaluated the effectiveness of defibrillation in public places found that the percentage of patients surviving after SCA was significantly higher when the help on the street was provided by bystanders trained to do cardiopulmonary resuscitation (CPR) using an automated external defibrillator (AED) (23%), compared with situations where only chest compressions were performed (14%) [10]. The comparable data were obtained when analyzing the real practice of AED installation in schools and police cars [11-13]. That is why in many countries in public places (pharmacies, stadiums, beaches, shopping malls, museums, tourist attractions, etc.), public transport, cars of law enforcement agencies and rescue services, the AEDs are installed; and also extensive training of medical workers, firefighters, rescuers, police officers, teachers, airline employees and just concerned citizens is carried out. In the UK, the BLS certification course (Basic Life Support — basic CPR using AEDs) is a prerequisite for obtaining a graduation certificate of middle school1. In Denmark currently it is mandatory for all drivers to hold a valid BLS certificate and therefore, as of January 1, 2020, 1 million out of 4,8 million people aged 15 to 105 years have been the trained providers of basic resuscitation [14]. As an experiment, some countries have pilot launched projects with the delivery of AEDs to the accident scene using unmanned aerial vehicles [15][16].
In our country, the currently existing legal limitations do not allow mass placement of AEDs in public places, since defibrillators are the medical devices, but it is possible within a medical facility. As for ambulatory subdivisions, taking into account the daily number of visits, many of them are actually a public place, and the availability of defibrillators and personnel capable of providing high-quality first aid increases the level of safety. According to the results of large-scale studies in Denmark and USA, it is economically reasonable to place the AEDs in areas where one cardiac arrest for a period from 2 to 5 years can be expected, and, for example, in Copenhagen, such a frequency of sudden cardiac arrests is recorded at train stations, in public parks and even pedestrian zones [17][18]. With a high degree of probability, it can be assumed that medical organizations also fall into this category. That is why, since the late 1980s, even before the introduction of public accessibility programs, AEDs were initially installed in hospitals and outpatient centers in various countries [19]. This practice is still quite common in the European region. For example, in Denmark, 93% of hospitals are equipped with AEDs, which are placed in public spaces, nonclinical subdivisions, usual hospital departments and are intended for use by personnel until the arrival of specialized resuscitation teams [19]. This strategy provides the best survival rates even in intrahospital cardiac arrest but only if the first discharge is applied no later than 3 minutes from the moment of calling for help [20].
To provide the work of all elements of the survival chain, in addition to the equipment, standardization of training of medical workers according to the algorithms adopted by the European Resuscitation Council (ERC) and the National Resuscitation Council (NRS) is extremely important [6][7]. The first step in the training system is the BLS protocol [21]. In foreign countries, the course of basic resuscitation is mandatory curriculum component of medical schools and universities [22][23]. The extended resuscitation programs — ALS (Advanced Life Support) in European countries or ACLS (Advanced Cardiac Life Support) — in the USA, UK and Canada are the mandatory component of residency training for doctors of all specialties [24].
The aim of the study: the present work is not a study in the classical sense; the authors tried to present and discuss their own experience of the AED accessibility program realization, implementing the training system for medical workers in concern with the Life Support strategy at different levels under oncological hospital conditions, as well as to identify those key points that should not be missed during the training, and difficulties that may arise during the implementation.
Material and methods
Since 2018 our medical organization (100-bed oncological hospital with departments of anesthesiology and intensive care, surgical oncology, general oncology and chemotherapy, radiation therapy, pediatric oncology; proton radiation therapy center with a 60-bed building; two outpatient polyclinic complexes with day hospitals; >80 free-standing diagnostic centers in the regions; nuclear medicine centers with a day hospital in Novosibirsk, Tomsk and Barnaul) has developed and has been implementing an AED accessibility program. The specificity of our organization is a large number of free-standing radiation diagnostic centers, where as a rule, there are only radiologists, radiologist technicians and medical registrars. In fact, they are the outpatient centers where, if necessary, the medical personnel have to provide the first and emergency care without any support of the resuscitation team and to call the city ambulance service therefore, it was necessary to train precisely these categories of medical workers.
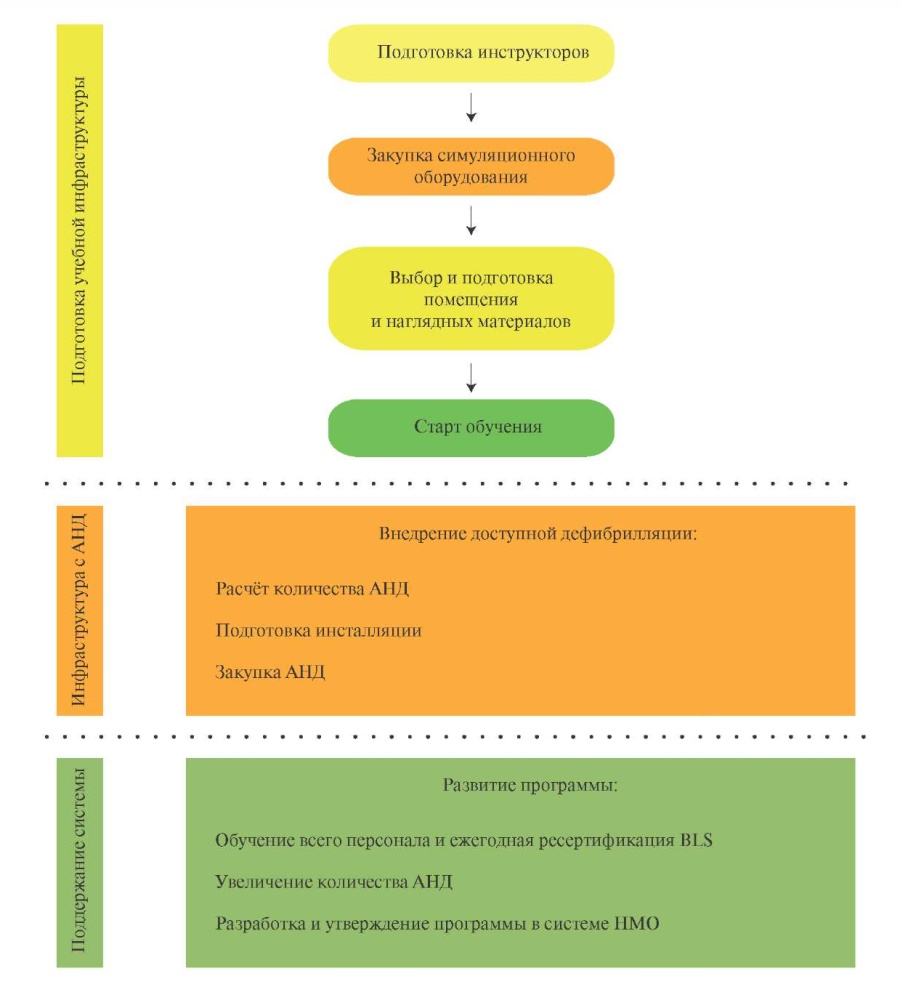
At the discussion of the conception stage, we developed a roadmap which has undergone many changes over these years, but today it can be presented as follows (Figure 1).

Figure 1. The stages of the implementing the program of accessible defibrillation.
Abbreviations: AED — automated external defibrillator, CME — continuing medical education, BLS — Basic Life Support.
As of 2018, there was only one NRS instructor working on a full-time basis, who, however, became the main organizer and motivator of the change implementation. Currently in Saint-Petersburg there are 890 employees in our organization (totally in the country >2000). Since, according to the ERS rules, the BLS training group consists of no more than eight students per a instructor, and the instructors are usually doctors who are primarily engaged in basic medical work, we had an urgent need for scale development of the simulation center. The purchase of equipment was carried out consistently, at the rate of one set per an instructor. The standard set for the basic resuscitation course includes a mannequin for simulating chest compressions and artificial inspirations (preferably with feedback), an Ambu bag, a training defibrillator, a vest for practicing manual skills of performing the Heimlich method. In our institution we used the mannequins Laerdal Resusci Anne QCPR of modification 2018, having a SkillGuide device to assess the depth, frequency of compressions and the effectiveness of artificial inspirations as well as the possibility to assess all these parameters with help of mobile application for smartphone, and also the training defibrillators Zoll AED plus and Philips Heartstart FRx.
The training is conducted by certified instructors in strict accordance with the training programs and clinical recommendations of the ERC and NRS. The training process is regulated by European Resuscitation Council: the class lasts 8 hours and includes theoretical blocks and practicing practical skills on simulators, both individually and at providing aid by two rescuers. From the moment of registration for the course until the course completion, the trainees receive the access to the course materials through an internal electronic platform — a course manual, videos, lecture material and a preliminary test task for self-preparation. The trainees who have successfully completed the practical exam issued the international certificate, and they receive the credit units in the system of continuing medical education (CME) in their personal account of the portal edu.rosminzdrav. To maintain skills and qualifications, the course should be repeated annually.
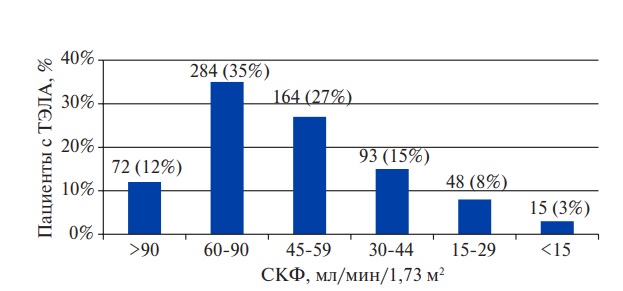
At the same time with the training, the concept of creating and promoting the infrastructure of the public-access AEDs was developed. At the initial stage, the main criterion to choose the addresses for AED installations was the presence of either department of anesthesiology and intensive care, or an anesthesiological group as well as the availability of outpatient consultations. Apart from that, a calculation method based on the data of NMRC named after A.N. Bakulev about the frequency of sudden coronary death in the Russian Federation amounting 150-450 thousand a year, i.e. approximately from 1 to 3 thousand per 1 million of population, was used. Thus, for example, if the patient flow through all oncological hospital subdivisions ~15 thousand people a year, there is a probability to meet approximately 15 sudden cardiac arrests hence, the AED installation appears reasonable. Since 2021, all the centers have been equipping with automatic defibrillators.
An extremely important point that can complicate the implementation of the defibrillator accessibility program is the choice of a source of financing for the purchase. The medical equipment standards of providing oncology and pediatric oncology medical care do not stipulate the availability of AEDs in the bed- and consultation departments. Therefore, a medical organization may purchase them either from extra-budgetary sources of financing or with the help of grants. Taking into account these specificities, both mechanisms were implemented in our organization — the first AEDs were purchased using own extra-budgetary funds of the hospital, then the grant support was received.
Results
In 2019-2022, 229 employees were trained according to the program (114 doctors, 85 specialists of the secondary medical staff and 30 non-medical workers). During the same period, after the first stage training, 15 doctors completed the ALS program, 3 doctors, 2 feldshers and 2 nurses — Immediate Life Support program, and 2 doctors — International Trauma Life Support program. Besides, 36 radiologists, medical physicists and radiotherapists passed the non-standardized first aid course under World Restart Heart Day (CPR skills using the AEDs) without obtaining a BLS certificate. The program was also implemented to the ambulatory oncologic centers in Novosibirsk, Barnaul, Tomsk (23 employees passed the program). The average age of all the trainees was 36,5 ages (from 21 to 66), 75 men and 154 women. The structure of the trainees is shown in the Figure 2.
Most of all the trainees were radiologists 38% (n=43), next — anesthesiologists-resuscitators 14% (n=16), and on the third place — heads of departments 9% (n=10).
As planned, a significant percent was occupied by the doctors of the radiology departments, since under the conditions of a free-standing office, it is the radiologist who, if necessary, will be the team leader and must possess all the required skills. A considerable number of anesthesiologists is explained by the mandatory successful passage of Advanced Life Support course in the trajectories of their professional development, and BLS is the first stage of ALS course.
In the composition of secondary medical personnel, 38% were occupied by radiologist technicians (n=32), and nurses and feldshers together — 62% (n=53). The non-medical workers were represented by medical registrars 50% (n=15), engineers 13% (n=4) and office workers — accounting department, etc. 37% (n=11).
Since only one instructor was involved in training for a long time, just over 70 employees completed the course between 2018 and the third quarter of 2021. Another limiting factor was the novel coronavirus infection pandemic, in which regulators limited the conduct of face-to-face educational events, and the ERC made changes to the BLS algorithm, structure and rules of the lesson. Apart from that, many doctor (including future instructors), radiologist technicians, nurses and registrars worked in repurposed centers for a long time; this excluded the very possibility of their participation in the training process.
With the improvement of the epidemiological situation, starting from October 2021, 3 people completed the course for instructors (BIC — Basic Instructor Course) and the traineeships necessary to obtain the status of a “full-fledged instructor”, additional simulation equipment was purchased, an electronic platform to register in the course with materials for self-training was created; all this made the possibility to abruptly intensify the process (Figure 3). The program itself became a resource for selecting potential instructors — during the course passage, the participants were evaluated, and the most active of them were invited to traineeships. Nowadays, the organization staff includes 4 fullfledged BLS instructors, 1 ALS candidate instructor and 1 International Trauma Life Support candidate instructor, but the development process of the simulation center continues, because the global goal is to train all employees without exception.
To harmonize the training program with the CME developmental strategy in 2022, we developed an additional professional education program “Basic Cardiopulmonary resuscitation of adults” (code V0002000-2022), which was examined and approved on the CME portal. Currently, medical workers are registered for the cycle and receive the credit units after successful completing the exam, that serves as additional motivation for them to pass the course. The development process is not complicated and is about the preparation of the training program itself, the creation of materials for the test exam, the creation of an electronic platform for trainees, where educational materials (lectures, videos, sample test assignment) are placed. An important point is that the program should be implemented not only through a full-time simulation course, but also with the participation of distance learning technologies and e-learning. Since basic CPR is included in the block of general medical knowledge, the program is intended (and is included in educational and methodological complexes) for doctors and nurses of all specialties.
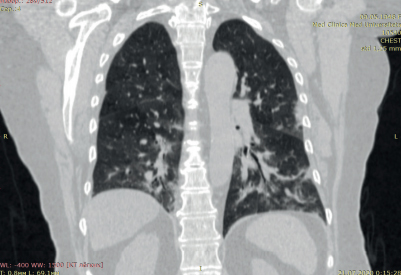
In addition to training, the second key point is the development of technical infrastructure of accessible AEDs. For the past 4 years, 12 AEDs have been installed in St. Petersburg and one in Novosibirsk, Tomsk and Barnaul. In Saint-Petersburg, they were installed in the greatest people concentration places and at the crossing of the main “routes” of staff and patients. This looks as follows: 3 defibrillators are placed in the oncological hospital (the hall of the first floor, the hall of the second floor, the registry of the radiotherapy building); 4 — in the proton radiation therapy center (the hall of the bed-building, the registry of the radiotherapy building, the hall of the day chemotherapy hospital, the hall of the positron emission tomography department), 3 — in outpatient departments, 1 — in the computed tomography center, 1 — in the magnetic resonance imaging center. The clinical subdivisions use Zoll AED plus, the free-standing diagnostic subdivisions — Philips Heartstart FRx. In accordance with European Resuscitation Council recommendations, each defibrillator is packed in a special bag containing reserve baby electrodes, sterile gloves, razors, gauze wipes, a breathing mask with a valve. The packing is placed in a wall cabinet with a transparent door and an identification mark. Above each cabinet with AED the signs indicating the emergency call number of the resuscitation team were mounted as well as a QR code that allows you to make an automatic call from a mobile phone by simply scanning with the built-in camera of a smartphone (Figure 4).

Figure 2. The structure of trainees according to profession/level of education.

Figure 3. Dynamics of the number of trainees by years (2022 — data for the first quarter).

Figure 4. The standard wall packing with AED.
In 2018-2022, there were three cases when first aid for SCA using AED was independently provided by medical workers of treatment and diagnostic departments before the arrival of the resuscitation team. In two cases they performed effective CPR; the rhythm was potentially defibrillable, and the application of the discharge restored the electrical activity of the heart, in one case there was a spontaneous restoration of the rhythm. Besides, in one case to eliminate airway obstruction, the Heimlich technique was used; in dozens of cases, after assessing the level of consciousness and the presence of breathing, patients were placed to a lateral recovery position. The implemented infrastructure also allowed to increase the mobility of resuscitators on duty, since currently there is no need to carry a defibrillator to the place of the first aid providing.
Because of the small number of cases with the use of AEDs, it is still quite difficult to fully assess the pharmacoeconomical effectiveness of the program implementation; at the same time, it is possible to estimate the level of costs, as well as to calculate the costs of one effective CPR.
1. The expenses for training.
Training of one instructor in the Moscow, St. Petersburg or Tomsk certified centers costs ~15 thousand rubles. It is required to have one set of the training simulators and devices for each instructor. The cost of BLS equipment depends on the manufacturer; the average cost of a set (a mannequin, a training defibrillator with consumable materials, a device for training Heimlich method) is ~100 thousand rubles. Apart from that, the organizational and administrative expenses (meals for trainees, since the ERC rules stipulate this, registration of a certificate, rental of premises, stationery, gloves, masks, etc.) are ~2 thousand rubles per a trainee in average. Thus, the final cost of the course, including amortization of equipment and payment of the instructor’s working time, ranges from 5 to 7,5 thousand rubles per a trainee. On one side, this seems large for the medical organization aiming to train all employees because these expenses are for hundreds of people. However, it is important to take into account that this course is a professional development, and if the program is approved in the CME system, the expenses for the training of medical workers may be taken from the compulsory medical insurance funds.
2. The expenses for the infrastructure of accessible defibrillation.
The cost of one AED Philips as 2021 is ~90 thousand rubles. The additional equipment (cabinet, packing, pediatric electrodes, etc.) raises main expenses up to 150 thousand rubles. Since currently AED are included in the equipment standards of only dental offices and ambulances, we have to find extra-budgetary sources of financing for infrastructure costs, and this, in our opinion, is the greatest organizational difficulty. Thus, the total costs for the program implementation for 4 years amounted to ~3,5 million rubles. In our case, the expenses for one effective CPR using AED when recalculating reached ~1 million rubles, which, in turn, is significantly lower than in foreign studies on pharmacoeconomics (the calculated QALY in which ranges from 30 to 50 thousand US dollars per defibrillator) [17].
Discussion
As the CME system has been gradually introducing in Russian healthcare since 2015, basic CPR has been included in the primary accreditation programs for all specialties [25]. At the same time, a medical worker passes primary accreditation only once, when receiving a specialty; hence, skills and knowledge that are not used in routine practice may be lost. That is why one of the ERC requirements is annual re-passing the BLS course [21]. This recommendation has a serious foundation and has been confirmed over the years by the results of various studies. Back in 2007, there was a study on a group of Birmingham University students, which evaluated the effectiveness of chest compressions on a mannequin with feedback directly during training and 6 weeks afterwards [19]. The obtained results were 58% and 43%, respectively. In 2021, the group of Spanish authors published the results of the study which evaluated the BLS knowledge survival among the students of medical colleges of the Almeria and Murcia universities [26]. The analysis included 479 trainees who were asked to undergo an assessment of theoretical knowledge and practical skills 6 months after completing the course. Only 60% of trainees showed satisfactory effectiveness of compressions (depth 67%, frequency 62,2%), and this allowed the authors to conclude that the training should be regular. For already working healthcare professionals, the situation may be even more critical. According to a multicenter study performed by Pakistani authors, the survival rate of skills among medical workers was 41,7% in average, and just 1 out of 140 respondents showed full knowledge of the BLS algorithm when tested [27]. At the same time, the study performed in the University of Pennsylvania showed that 6-11 months after the course completing the level of manual skills falls up to 74%, while in the period from 12 to 17 months — up to 71%, that looks quite optimistic [28]. In general, the majority of studies accepts that the training process should be constant and repetitive. In our opinion, it is the regular annual simulation training that allows medical professionals to make the correct algorithm of actions when meeting SCA. Undoubtedly, continuous training and regular re-certification require significant resources, but this is the only way to develop and maintain CPR skills using the AEDs.
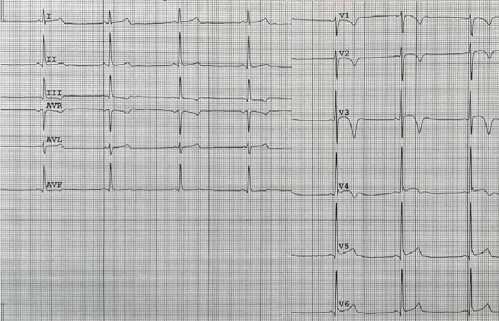
An interesting issue is reasonability of the implementing automated defibrillation in a medical facility. At first glance, especially in the buildings having the anesthesiology-resuscitation departments or groups, this step seems excessive. However, the standard practice, including the world experience, shows that while meeting a patient with SCA, some time is spent on calling a duty doctor, then some time is spent on calling a resuscitator, and as a result, precious minutes are lost for the delivery of a manual defibrillator and the arrival of a specialist who is able to assess the patient’s condition and adequately carry out resuscitation measures [20][29]. Apart from that, the important restriction in use of biphasic defibrillator monitor (even if it is available in quick access) in manual mode is the fact is that rhythm assessment and decision-making for manual defibrillation require good skills to quickly read an electrocardiogram from a monitor screen, which is not always applicable to doctors and nurses of those specialties that do not involve daily work with an electrocardiogram. One of the solutions in Western hospitals was the formation of the so-called Code team — emergency resuscitation teams of doctors and nurses who are not employees of intensive care units, but have been certified for advanced resuscitation measures [30]. At the same time, the availability of such teams requires significant resources both for training and for the infrastructure development (resuscitation trolleys with defibrillators and packing of drugs and medical devices), that may not always be implemented in all departments. Thus, the ERC experts recommend to use AEDs in semi-automated mode in those hospital departments where is the risk of the delay of defibrillation for several minutes (more than 2-3 min), and where the workers who first react to SCA do not have an experience of manual defibrillation [21, 31, 32]. In general, intrahospital SCA are characterized by low survival rate which ranges within 10-20% [20]. If in the intensive care units this situation is explained by the structure of electrical rhythms of arrest (the predominance of potentially non-defibrillable arrests — electromechanical dissociation and asystole), then in usual departments and public places of hospitals, the leading cause is delayed defibrillation [20]. That is why until now the practice of mass training of medical personnel and the installation of automated defibrillators is recognized by most researchers as adequate [20][29].
As for free-standing units, the problem is even more acute, since qualified help in this case involves the call and arrival of an ambulance team. Even with strict time standards for the arrival of the brigade in megacities (~20 min) and the early start of chest compressions, the time interval before the first discharge can be tens of minutes, which negatively affects the further prognosis of patient survival. Psychological barriers, especially in secondary medical personnel, are also important moment. According to the results of the published in 2018 multicenter research, which carried out in three Canadian university clinics, 87,5% of nurses performed CPR at least once in their life but only 29% of them used defibrillator [29]. That is why in our practice, at the first stage, we concentrated on training nurses and radiologist technicians. Undoubtedly, the global goal — to train all employees — has not yet been achieved, but after 4 years of implementation, it became obvious to us that it is achievable.
Conclusion
The implementation and development of the AED accessibility program in combination with the training of personnel under the Life Support programs, is a useful and necessary process under the conditions of a medical organization. The employees trained to perform the measures of first and emergency care according to the standards, and the presence of the corresponding material and technical base form a certain safety culture.
The doctors and nurses who successfully passed the basic resuscitation course are the personnel reserve for the training extended resuscitation measures, the formation of emergency resuscitation teams and the expansion of the teaching staff of the simulation center.
Acknowledgments. The authors would like to thank Z.A. Zaripova for methodological support in the training of coaches, and A.O. Marichev for his contribution to the training system management.
Relationships and Activities: none.
1. Education and Training (Welfare of Children) Act 2021. 29 April 2021. https://www.legislation.gov.uk/en/ukpga/2021/16/enacted (доступ 26.04.2022).
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Cherkashin M.A., Nikolaev A.A., Berezina N.A., Berezin N.S., Bolshakova T.V. Experience in implementing a program for basic life support and available automated defibrillation in a cancer center. Russian Journal of Cardiology. 2022;27(3S):5065. https://doi.org/10.15829/1560-4071-2022-5065
Copy