Optimal management of patients with ST-segment elevation myocardial infarction with delayed admission to the percutaneous coronary intervention center (more than 12 hours)
Coronary artery disease (CAD) is one of the leading causes of death, while the maximum mortality among all CAD types is observed in patients with ST segment elevation myocardial infarction (STEMI). According to statistics, 508,6 thousand people died from CAD in Russia in 2020 [1]. MI can become the debut of CAD or be its manifestation in persons with an already established diagnosis [2]. The success of treating such patients largely depends on the timely provision of specialized health care, primarily on the restoration of blood flow through the infarctrelated artery (IRA), which must be achieved within a minimum period from the onset using a drug or invasive strategy. However, STEMI patients are far from always admitted to specialized centers performing percutaneous coronary intervention (PCI) in the early period, while hospitalization of a patient more than 12 hours after the symptom onset is a predictor of an unfavorable outcome and indicates a high death risk. If a patient is admitted with STEMI >12 hours from the onset of myocardial ischemia, thrombolytic therapy is not used, and PCI is used as a method of revascularization. However, it is precisely such patients in actual clinical practice that are often treated conservatively.
To date, several registries have published data suggesting that delayed revascularization (>12 h from symptom onset) performed in STEMI patients leads to improved survival in both the short and long term periods [3-5]. This fact can be explained by the open-artery hypothesis proposed by Kim CB and Braunwald E, according to which even a rather late restoration of blood flow through the occluded artery reduces the severity of postinfarct remodeling and improves long-term patient outcomes [6].
In the current version of ESC/EACTS guidelines on myocardial revascularization (2018), the routine primary PCI in patients hospitalized >12 hours from the symptom onset reaches IIA class of recommendations, which means the presence of conflicting evidence and/or divergence of opinion about the usefulness/efficacy of the given procedure, while most of the evidence/opinion is in favor of usefulness/efficacy [7].
Given the low clarity regarding the treatment tactics for STEMI patients who were admitted within 12-48 hours after the symptom onset, we reviewed the available literature sources that studied the outcomes of such patients depending on the invasive or conservative management strategy, as well as a retrospective analysis of the data from Samara Regional Registry for Acute Coronary Syndrome for 2013-2018.
Material and methods
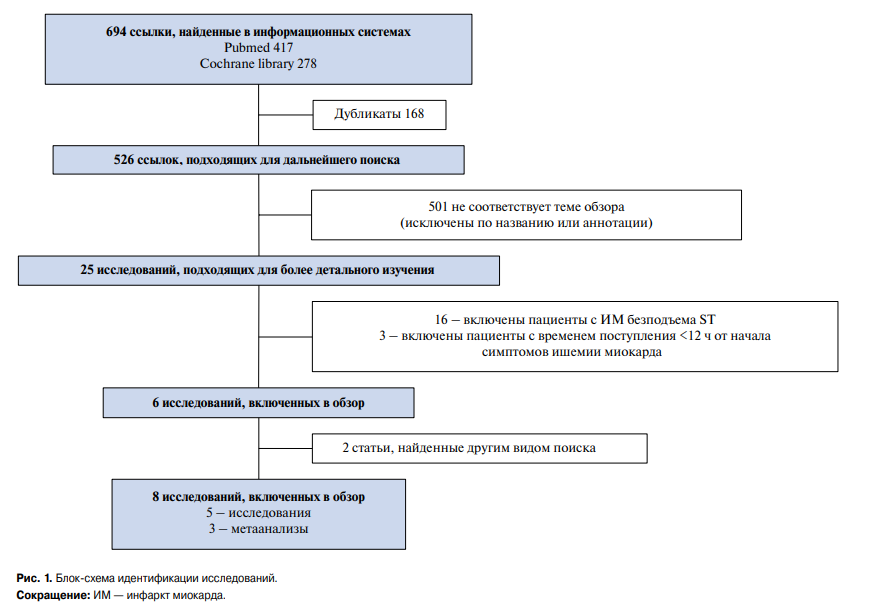
The review study was conducted from September 2019 to May 2020. The search was carried out in the following databases: PubMed, Cochrane library. We used following keywords: acute myocardial infarction, ST segment elevation acute coronary syndrome, percutaneous coronary intervention, revascularization. There were following inclusion criteria: randomized distribution into treatment groups, comparison of PCI versus conservative management, hemodynamic stability of patients, PCI of fully occluded IRA performed >12 h after the onset of myo – cardial ischemia symptoms. As a result, 8 studies met the criteria of our review, of which 5 were clinical studies and 3 — meta-analyzes (Figure 1). To date, a small number of studies have been conducted to study the rationale for late PCI in STEMI, and the data obtained are contradictory.

Figure 1. Flow chart of study identification.
Abbreviation: MI — myocardial infarction.
Research review
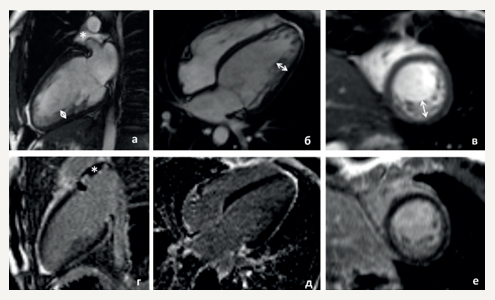
The BRAVE-2 study (2005) [8] assessed both short-term and long-term outcomes in patients admitted with STEMI 12-48 hours after the symptom onset, depending on the treatment strategy. This study included 365 STEMI patients who were admitted late from the symptom onset. Patients were randomized to the invasive group (n=182) and the conservative group (n=183). The follow-up period lasted 4 years. At the first stage, the final left ventricular (LV) infarct size was considered as the primary endpoint, which was assessed using single-photon emission computed tomography immediately after randomization and after 5-10 days. Statistical analysis showed that invasive strategy in patients admitted with STEMI >12 h after symptom onset is associated with preserving some degree of myocardial viability and a decrease in the final LV infarct size. According to the results obtained, the final LV infarct size was significantly less in patients in the invasive group compared with the conservative group — 8,0% (2,0-15,8) and 12% (3,2-25,0) of LV size (P=0,004). The preserved myocardium index was 0,44 (0,13-0,8) in the invasive group versus 0,23 in the conservative group (0,0-0,5); P<0,001. At the second stage of the BRAVE-2 study, the incidence of death due to cardiovascular causes, MI, stroke, and the need for revascularization were assessed. In the group of patients who underwent PCI, death occurred in 20 patients (11,1%; 95% confidence interval (CI), 7,3-16,7) un the invasive group, and in 34 patients (18,9%; 95% CI, 13,9-25,4) in the conservative group (unadjusted hazard ratio (HR), 0,57; 95% CI, 0,33-0,99; P=0,047; adjusted HR, 0,55; 95% CI, 0,31-0,97; P=0.04). The 4-year incidence of MI and stroke did not differ between the groups: MI occurred in 12 patients (6,8%; 95% CI, 3,9-11,7) in the invasive group and in 10 patients (5,6%; 95% CI, 3,0-10,1) in the conservative group (unadjusted HR, 1,20; 95% CI, 0,52-2,78; P=0,66); stroke developed in 3 (1,6%) and 2 (1,1%) patients in the invasive and conservative groups, respectively (P=0,65). Subsequent revascularization of IRA was performed in 45 patients in the invasive group, while in the conservative management group — in 125 patients (25,8% vs 69,1%; P=0,001). The authors conclude that PCI even at a later time (>12 hours after the onset of myocardial ischemia symptoms) not only preserves myocardial viability, but also improves the long-term prognosis, reducing the incidence of cardiovascular complications and reducing mortality in the invasive group [3].
Purpose of the study by Gierlotka M, et al. (2011) was to investigate whether reperfusion in primary PCI improves 12-month survival in STEMI patients with late admission. Data from the Polish registry of acute coronary syndromes (PL-ACS) were used. The information was collected by qualified physicians, and initially 23517 STEMI patients who were admitted to hospitals between June 2005 and August 2006 were included in the analysis. There were following exclusion criteria: cardiogenic shock, pulmonary edema, thrombolysis. As a result, we analyzed the data of 2036 patients with STEMI who were admitted within the period from 12 to 24 hours after the onset of myocardial ischemia symptoms. Patients who underwent coronary angiography during this time period were included in the invasive group, which consisted of 910 (44,7%) people (92% of them underwent reperfusion by PCI). All other patients who received only drug therapy or coronary angiography performed 24 hours after the symptom onset were included in the conservative group. After 12 months, the following outcomes were assessed: all-cause, recurrent myocardial infarction, stroke. In patients with an invasive approach, there was a significant decrease in 12-month mortality, compared with patients with a conservative approach (9,3% vs 17,9%; P<0,0001). The main conclusion of this analysis is that the current invasive methods for STEMI patients, despite their late admission, leads to a decrease in 12-month mortality compared with the conservative approach [4].
The paper by Fan Y, et al. (2015) studied patients with STEMI who were hospitalized in the period from 2009 to 2011 in PCI centers. In total, the analysis included 1090 patients who either underwent delayed PCI (n=786), or received only standard drug therapy (n=304). PCI was considered delayed if the symptom-onset-to-balloon time was >24 h. Exclusion criteria were idiopathic cardiomyopathy, congenital heart defects, valvular heart disease, rheumatic or autoimmune diseases, cancer, severe liver or kidney dysfunction, or other uncontrolled systemic diseases, as well as the impossibility of PCI. The primary endpoint included adverse cardiovascular events such as all-cause and cardiovascular deaths, readmission for heart failure (HF), readmission for angina, recurrent nonfatal MI, recurrent coronary revascularization, and stroke. Echocardiographic characteristics of LV remodeling were studied. Initially, these parameters did not differ in the compared groups. The mean follow-up period was 36 months. In the conservative group, LV remodeling was more pronounced than in the group of patients undergoing delayed PCI. Patients in the conservative group had a larger LV diameter, volume and mass, as well as more pronounced LV contractile dysfunction. Statistical analysis using logistic regression showed that delayed PCI independently and negatively correlated with LV remodeling (odds ratio, 0,356; 95% CI, 0,251 0,505; P<0,001). The Kaplan-Meier analysis showed a lower risk of major adverse cardiovascular events, all-cause death, and rehospitalization for decompensated HF in the delayed PCI group compared with the conservative group [5].
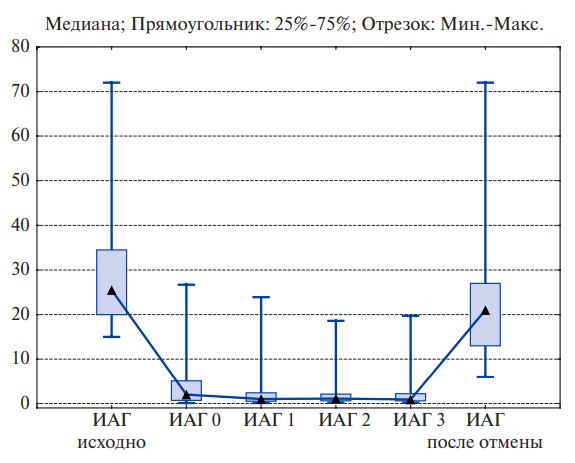
The TOSCA-2 study (2006) assessed the PCI effect on myocardial contractility and remodeling in stable patients who had undergone STEMI from 3 to 28 days ago. The LV ejection fraction (LVEF) and the end-systolic (ESV) and diastolic volumes (EDV) were assessed 1 year after randomization. In the period from May 2000 to July 2005, patients with occluded native IRA (n=381) were randomized into two groups of PCI with stenting and conservative therapy. Repeated coronary angiography and LV angiography were performed 1 year after randomization (n=332, 87%). As endpoints, we analyzed the IRA patency, changes in LVEF, ESV and EDV. At the end of follow-up period, there was a significant increase in LVEF (P=0,001) in both groups compared to the baseline values, without intergroup differences: PCI, 4,2±8,9 (n=150) vs drug therapy, 3,5±8,2 (n=136; P=0,47). The median change (interquartile range) in LV ESV index decreased by 0,5 ml/m2 (9,3-5,0) in the invasive group versus an increase by 1,0 ml/m2 (5,7-7,3) in the drug group (P=0,1). The median change in the LVEF index reached 3,2 (8,2-13,3) vs 5,3 (4,6-23,2) ml/m2 (P=0,07) in the PCI groups (n=86) and drug therapy (n=76), respectively. The study revealed a trend towards improvement of studied parameters in STEMI patients with delayed admission undergoing PCI. However, these differences did not reach statistical significance [9].
Abbate A, et al. (2008) performed a meta-analysis of ten randomized trials comparing the survival of hemodynamically stable patients in the PCI and conservative groups with delayed admission to a specialized hospital. The total number of patients was 3560. The follow-up duration ranged from 42 days to 10,2 years (on average, the median follow-up was 2,8 years). Patients were divided into PCI (n=1779) and conservative groups (n=1781). The number of deaths was 112 (6,3%) and 149 (8,4%), respectively, which indicates a significant improvement in survival in the PCI group (odds ratio, 0,49; 95% CI, 0,26-0,94; P=0,03). In addition, an increase in LVEF was found in the PCI group by 4,4% (95% CI, 1,1-7,6; P=0,009) compared with the conservative group. Thus, the results of statistical analysis showed that surgical management was associated with a better prognosis and led to LVEF increase in patients with MI within prior 3-28, in comparison with drug therapy [10]. The study limitations are a significant variation in the time elapsed from the symptom onset (12 hours — 60 days), and the lack of data on optimal PCI timing.
Appleton DL, et al. (2008) prepared a metaanalysis of five studies, which included a total of 648 patients as follows: PCI group — 342, conservative group — 306. According to the work, there was a significant difference in LVEF increase in favor of the PCI group (+3,1%, 95% CI, 1,0-5,2, P<0,0004). In addition, significant differences were found in changes in both LV EDV (5,1 ml higher decrease in PCI, 95% CI, -9,4 — -0,8; P=0,02) and LV ESV (5,3 ml higher decrease in PCI, 95% CI, -8,3 — -2,4; P=0,0005). The authors concluded that delayed revascularization of occluded IRA can improve myocardial systolic function and reduce the severity of its remodeling, which supports the openartery hypothesis mentioned earlier [11].
The meta-analysis by Hai-Tao Yang, et al. (2019) evaluated 18 studies involving 14677 patients, of which 5157 received delayed PCI and 9520 — drug therapy. This analysis included randomized controlled trials as well as observational and cohort studies, where patients with MI underwent delayed reperfusion (>12 h) or received conservative therapy. The mean follow-up period lasted 12 months. The authors compared outcomes such as all-cause mortality, adverse cardiovascular events, and HF decompensation in the conservative and delayed PCI groups. The analysis found that delayed PCI was associated with a decrease in all-cause mortality (HR, 0,60; 95% CI 0,44-0,83; P=0,002), major adverse cardiovascular outcomes (HR, 0,67; 95% CI, 0,50-0,89; P<0,001) and HF (HR, 0,76; 95% CI, 0,60-0,97; P=0,03) compared with drug therapy. There was also a trend towards a decrease in MI recurrence in the invasive group (HR, 0,70; 95% CI, 0,47-1,05; P=0,08). At the same time, delayed PCI significantly improved the outcomes only if it was performed within 12-48 hours from the symptom onset, while revascularization at a later time (2-60 days) did not have a favorable effect [12].
The OAT study (2006) is one of the papers that indicate no benefits in long-term outcomes in patients received PCI within 3-28 days after the onset of myocardial ischemia symptoms with occluded IRA. From February 2000 to December 2005, this study included patients (n=2166) with total IRA occlusion who were admitted within 3-28 days from the symptom onset. Patients with NYHA class III-IV heart failure, shock, creatinine level >221 ?mol/L, severe left coronary artery trunk involvement or three-vessel disease, unstable angina, severe ischemia detected during the exercise stress test were excluded. Patients were randomized to PCI (n=1082) and drug management (n=1084) groups. The primary endpoint was a combination of all-cause death, MI, hospitalization for NYHA class IV HF. The median follow-up was 2,8 years. Ultimately, planned outcomes were observed in 161 versus 140 patients in the invasive and conservative groups, respectively. The overall incidence of primary endpoint over 4 years was 17,2% in the PCI group versus 15,6% in the conservative management group (HR, 1,16; 95% CI, 0,92-1,45; P=0,20). MI incidence between the groups also did not differ, amounting to 7,0% in the PCI group versus 5,3% in the conservative group (HR, 1,36; 95% CI, 0,92-2,00; P=0,13). The incidence of NYHA class IV HR was 4,4% in the invasive group and 4,5% in the conservative group (P=0,92). Mortality from various causes — 9,1% and 9,4% in groups, respectively (P=0,81). The authors concluded that the effectiveness of PCI in stable patients with occluded IRA, admitted within 3-28 days from the symptom onset, is comparable with the optimal conservative therapy [13].
For the combined analysis of publications included in the review, it was possible to use 11 studies, since they contained the necessary detailed data. The total number of patients was 15038. The invasive group included 5660 patients, while the conservative group — 9378. Major adverse cardiovascular events such as death, MI, HF-related hospitalization were selected as the composite endpoint. These outcomes were significantly higher in the conservative group (12,6%) compared with the invasive group (9,2%) (HR, 1,3; 95% CI, 1,2-1,5; P<0,05).
Table 1 presents a list of studies included in the meta-analyzes and a review on this topic, indicating the main cohort characteristics, the follow-up duration and results obtained.
Table 1
Characteristics of the studies


Note: * — differences are statistically significant (р?0,05).
Abbreviations: CI — confidence interval, MI — myocardial infarction, IRA — infarct-related artery, EDV — end diastolic volume, ESV — end systolic volume, LV — left ventricle, HR — hazard ratio, HF — heart failure, MACE — Major adverse cardiovascular events, EF — ejection fraction.
Given the conflicting data on benefits of invasive procedure in STEMI patients who were admitted to the PCI center 12-48 hours after the symptom onset, we conducted a retrospective analysis of data from Samara Regional Registry for Acute Coronary Syndrome for 2013-2018.
Results
During mentioned time period, the number of STEMI patients who were admitted 12-48 hours after the onset of myocardial ischemia symptoms was 606. Further, patients with following characteristics were excluded from the analysis: with indications for primary PCI, with severe comorbidities, with indications for direct oral anticoagulant therapy; those who received a thrombolytic agent in an index hospitalization, persons over 80 years old. As a result, the study population was 258 people. The mean age of patients reached 60±11 years. The patients were divided into two groups depending on the initially selected management strategy: invasive (I) and conservative (II) groups. Patients of group I, in addition to optimal medication therapy, underwent coronary angiography followed by IRA revascularization (n=193; 74,8%). Group II received only optimal drug therapy, without PCI (n=65; 25,2%). Mortality during the hospitalization was analyzed. This parameter was significantly higher in group II (7,9%) in comparison with group I (0,5%) (HR, 14,8; 95% CI, 1,7-124,7; P<0,05).
Thus, the results of our study showed that the invasive strategy improves in-hospital survival in STEMI patients admitted within 12-48 hours after the symptom onset. These results are consistent with a number of works described above [3-5][10][12].
Discussion
An analysis of the works presented in this review indicates that most authors have established a beneficial effect of delayed PCI on patient survival, the incidence of cardiovascular events, and the severity of myocardial remodeling.
It should be especially noted that in presented studies, there were no uniform criteria according to which patients were included in conservative and invasive groups. A number of authors included in the invasive group not only those patients who underwent stenting of IRA, but also patients who underwent only coronary angiography. In other studies, performing coronary angiography was considered a diagnostic procedure. In our opinion, it is more correct to classify patients who underwent only coronary angiography without subsequent stenting into the conservative group. Also, in many studies, there was no clarity on PCI timing.
The improvement in life prognosis in STEMI patients with delayed admission after PCI can be attributed to several reasons. First, a viable myocardium in the IRA system can persist even after 12 hours from the symptom onset, while revascularization of IRA has a beneficial effect on hibernating cardiomyocytes, even if it occurs quite late and goes beyond the standard period established for myocardial revascularization before necrosis development [6]. Second, even delayed reperfusion accelerates the healing process of tissues after MI, during which many infiltrating cells can play a significant role in collagen synthesis and lysis of necrotic myocardium. Late reperfusion not only promotes the proliferation of cardiomyocytes, but also protects them from apoptosis [14]. Third, collateral circulation is one of the factors that maintain coronary flow at the level necessary to maintain myocardial viability after coronary occlusion, which specifies the potential for LV functional restoration after delayed mechanical reperfusion [15-17].
There were a number of limitations of our review. The inclusion criterion in this review was complete occlusion of IRA, while the results of this publication do not apply to the patients with delayed spontaneous recanalization. Several published studies included in meta-analyzes did not detail the data. In the BRAVE-2 study, abciximab was also used in the PCI group, which should be considered.
Conclusion
Thus, most of the literature sources analyzed indicate that invasive management of STEMI patients admitted to the PCI center 12-48 hours after the symptom onset improves in-hospital and long-term prognosis. Our retrospective analysis showed improved survival during the hospitalization period. On the one hand, the pathophysiological mechanisms underlying this phenomenon have been described in sufficient detail. On the other hand, several studies have been published that do not support the PCI benefits in this category of patients. Moreover, to date, there is no unambiguous opinion about the timing during which PCI improves the prognosis of patients if they are admitted >12 hours from the symptom onset. It seems appropriate to conduct a prospective randomized study to finally determine the effect of delayed PCI on patient outcomes and to determine the time period during which invasive treatment significantly increases the survival rate in these patients.
Relationships and Activities: none.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Vorontsova S.A., Pavlova T.V., Khokhlunov S.M., Podlipaeva A.A. Optimal management of patients with ST-segment elevation myocardial infarction with delayed admission to the percutaneous coronary intervention center (more than 12 hours). Russian Journal of Cardiology. 2021;26(3S):4518. https://doi.org/10.15829/1560-4071-2021-4518
Copy