ICD-10 code-based definition of heart failure in Saint Petersburg electronic health records: prevalence, health care utilization and outcomes
Heart failure (HF) significantly contributes to premature disability and mortality [1]. Despite the high and growing prevalence of HF in Russia [2][3], there are no accurate epidemiologic data in regions and the country as a whole, which emphasizes the relevance of large-scale epidemiological studies.
With the healthcare system modernization, medical information systems and electronic medical records are becoming an accessible and informative resource of health characteristics of a large population group, including about the HF epidemiology. However, the informatization level in Russian subjects varies significantly, and the information about symptoms, levels of left ventricular ejection fraction (LVEF) and natriuretic peptides, necessary for objectifying the HF diagnosis, is not systematically collected. To date, to obtain data on HF prevalence, assessment of coding according to the International Classification of Diseases, Tenth Revision (ICD10) in medical records seems to be the most effective. Although the main ICD-10 code for HF is I50.x, large-scale foreign studies and national registries use additional codes that potentially characterize HF [4-7]. Acceptable sensitivity and high specificity of this approach in HF detection [8] allows it to be used as an initial step in the study of its epidemiology.
The aim was to analyze HF prevalence, clinical and demographic characteristics, health care utilization, and outcomes according to the used International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD10) codes in regional integrated electronic health record database in Saint Petersburg.
Material and methods
A retrospective analysis of the regional integrated electronic health record database received from 250 state medical facilities of Saint Petersburg in 2019 was performed. The database covers the entire city population, contains information about ~95% of deaths and ~65% of admissions to all medical organizations. The analysis was performed among the adult population. The final data was obtained by structured queries. At least one of the following ICD-10 codes has been considered as HF case: I09.9, I11.0, I13.0, I13.2, I25.5, I42.0, I42.5, I42.6, I42.7, I42.8, I42.9, I43.0, I43.1, I43.2, I43.8, I50.x (Table 1) [8]. To assess HF prevalence, we assessed the working-age and elderly population in Saint Petersburg at the beginning of 2019 according to data from the Federal State Statistics Service [9]. Age and sex characteristics of HF patients, comorbidities, frequency of medical encounters, and all-cause mortality were assessed. To study patient characteristics, depending on the established ICD10 code, the entire contingent was divided into the following groups: standard coding — I50.x, extended coding — I11.0, I13.0, I13.2, I25.5, I42.0, I42.9, I09.9, I43.0, I43.1, I43.2, I43.8, I42.5, I42.6, I42.7, I42.8. The processed data were presented as absolute numbers and proportions.
Table 1
ICD-10 codes used in the study
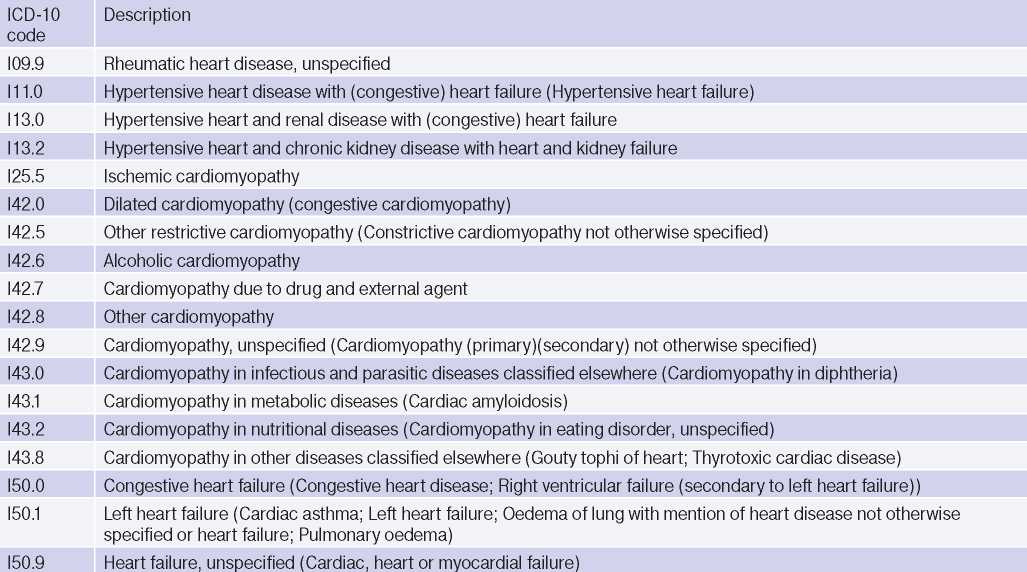
Abbreviation: ICD-10 — International Classification of Diseases, Tenth Revision.
The study was performed in accordance with Good Clinical Practice and Declaration of Helsinki.
Results
In 2019, in Saint Petersburg, 64070 adult patients with HF had medical encounters (men, 32,4%; age over 60, 73,3%). Standard coding identified 34,5% of HF patients, while extended coding — 65,5%. A combination of codes was observed in 9,9% of patients (Figure 1). Standard coding prevailed in hospitals, while extended coding prevailed in outpatient clinics (Figure 1). The HF prevalence was 1,4% (or 14,1 per 1000 population), while mortality — 6,8%.
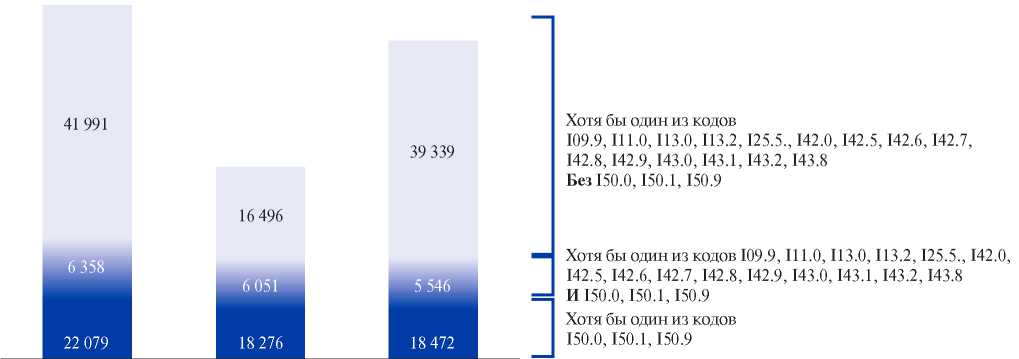
Figure 1. Number of patients included in the analysis, depending on the established codes and on the conditions of care.
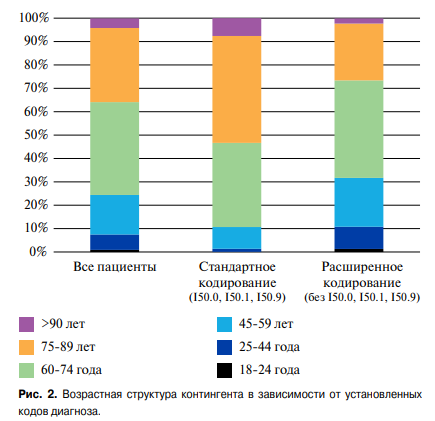
In addition, standard coding revealed HF prevalence and mortality in Saint Petersburg in 2019 of 0,49% and 15,7%, while extended coding — 0,93% and 2,1%. Standard versus expanded coding identified older patients (87,8% over 60 years of age vs 65,6% (Figure 2)), more males (39% vs 29%) and a higher incidence of comorbidities except for hypertension and cardiomyopathy (Figure 3).
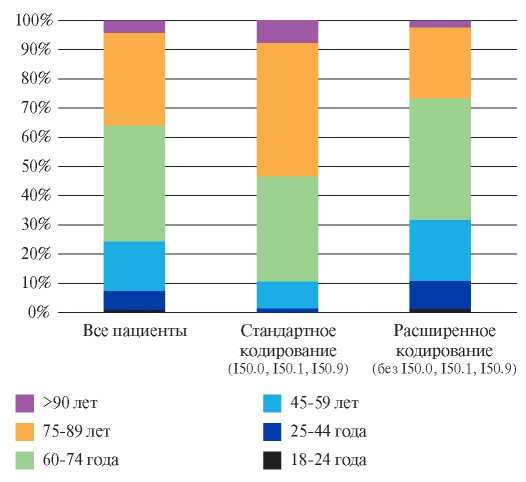
Figure 2. Age pattern of the contingent depending on the established codes.
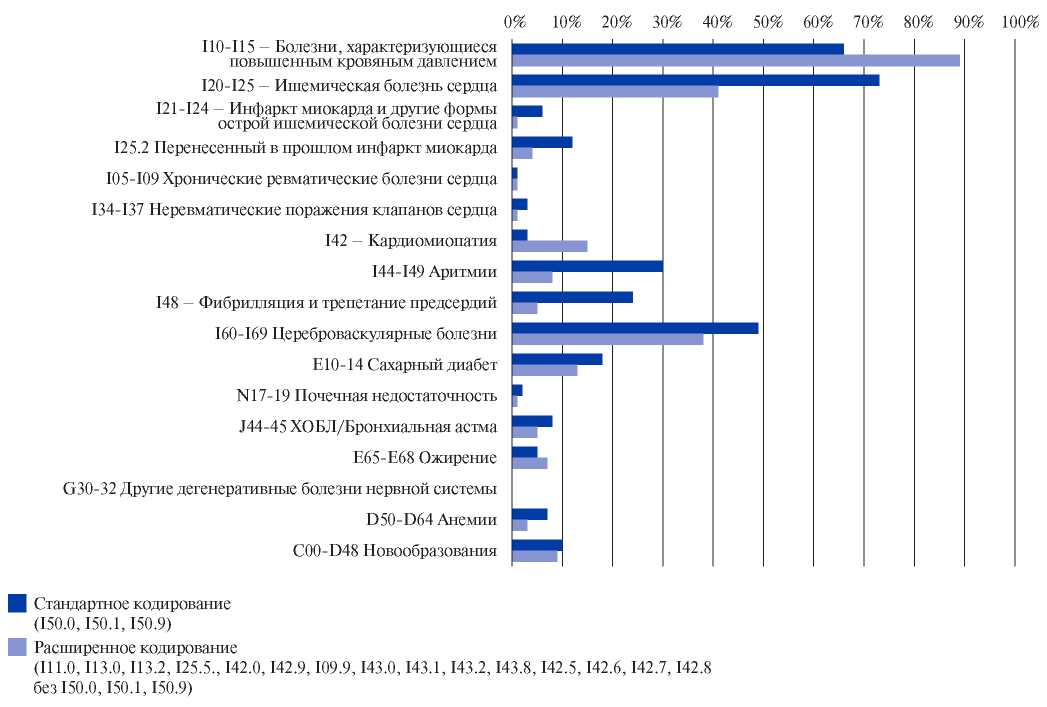
Figure 3. Frequency of related codes in the diagnosis depending on the established codes.
Abbreviation: COPD — chronic obstructive pulmonary disease chronic obstructive pulmonary disease.
Among all medical encounters in Saint Petersburg in 2019, the proportion of HF-related visits was 4,3% in total, 6,5% — among all hospitalizations, 4,1% — among all visits to outpatient facilities, 9,7% — among all emergency calls. HF patients were characterized by a high frequency of medical encounters as follows: an average of 14 visits per patient per year. In addition, 24% of patients had >20 visits per year, and 54% had at least one hospitalization for any reason during the year. Within the groups, there was a comparable high, but structurally different, burden on healthcare system. In the standard coding group, compared to the extended group, there were more hospitalizations (1,4 vs 0,6 per patient), emergency calls (1,2 vs 0,5 calls per patient), and a higher proportion of patients without outpatient visits during the year (16,3% vs 6,3%).
Discussion
An accurate regional and global assessment of the disease burden is key to setting treatment priorities, preventing complications, identifying needs, planning the use of health system resources, and research. The peculiarities of HF statistics, combined with the heterogeneity of this syndrome, limit obtaining accurate epidemiological information about the disease both in Russia and in the world [10]. In the presented real-world evidence study, using a large-scale regional database, for the first time in Russia, an analysis of HF prevalence was performed based on ICD-10 codes. HF-related burden on health system, the mortality rate, as well as differences between groups depending on codes were studied. The extended ICD-10 coding revealed the HF prevalence in Saint Petersburg of 1,4% (or 14,1 per 1000 population), annual mortality of 6,8%. It has been established that patients with HF account for 4,3% of all medical encounters.
Currently, there are >64 million patients with HF in the world, or 0,8% of the total population [6]. However, data from different countries vary significantly in terms of established rates and methods of data collection [6][7]. In the Global Burden of Disease study, the age-standardized prevalence of HF in Russia in 2017 was 6,94 (6,02-7,95) per 1000 population compared to 10,58 (9,26-12,04) in the central Europe [6]. According to the EPOHA epidemiological studies performed at the out- and inpatient stages in 8 Russian subjects, HF prevalence in Russia in 2017 was 3,1-10,4%, depending on the diagnostic criteria used [3]. According to additional analysis, the estimated prevalence of HF in the European Russia was 7% [11]. It should be noted that the obtained values are significantly higher than the estimated HF prevalence in USA (2,4-2,6%), Canada (3,6%), China (1,3-3,5%), Australia (1,2- 5,3%) and most European countries [6][7][12][13].
Our study of HF prevalence in Saint Petersburg, based on the coding in routine clinical practice, is simple in methodology, which is consistent with similar epidemiological studies abroad. This allows us to compare the results with data on other Russian subjects or other countries. In the meta-analysis of 11 studies, with high specificity (96,8%), HF detection using ICD codes had a low sensitivity of 75,3% (95% confidence interval, 74,7-75,9) [8]. This suggests that at least a quarter of HF cases could have been left unrecorded in our study, and we can expect an estimated prevalence of HF in Saint Petersburg at a level of up to 18,8 per 1000 population. The resulting number is comparable to the European average, established according to the HFA Atlas project initiated in 2018, where the median HF prevalence in 13 European countries in 2019 was 17,2 (14,3-21,0) per 1 thousand population, varying from ?12 in Greece and Spain to >30 in Lithuania and Germany [12].
Undoubtedly, the presented approach to assessing the HF epidemiology cannot be considered as a reference one, since it largely depends on electronic medical records and a particular doctor’s choice of diagnosis codes. We have shown that only a third of HF cases are verified using the ICD-10 code I50.x. In the Finnish registry on HF, the majority of patients were included in the primary cohort with the I50.x code, while only 7,6% were included in the codes for cardiomyopathies or hypertension [14]. Perhaps the presented differences are related to the analysis of entire clinical practice performed in our case, including primary care physicians or doctors of other specialties, or to national characteristics of coding and overdiagnosis of HF in risk groups. There are also differences depending on the stage of care, since I50.x code is more often used in a hospital. Of particular difficulty is the analysis of the prevalence of HF with preserved EF (HFpEF), when the risk of overdiagnosis is high. According to a small Russian study, the HFpEF diagnosis made by a hospital doctor was not confirmed using modern diagnostic criteria in 63% of cases [15]; according to the European HF registry — in 52% of cases [16]. At the same time, it is practically impossible to use HF criteria proposed in the clinical guidelines for epidemiological purposes, since this requires simultaneous interpretation of clinical and echocardiographic signs, as well as an assessment natriuretic peptide in patients with LVEF of 40% or more [1]. Such information is not widely available or routinely measured. Thus, in the Finnish HF registry, LVEF values were available only in half of the cases [17]. A recent study of 888 outpatient records of HF patients in 7 Russian regions demonstrated that in actual clinical practice, the level of N-terminal probrain natriuretic peptide (NT-proBNP) is determined only in 1% of cases [18].
A significant step towards the uniformity of HF verification was the publication of Universal Definition of Heart Failure [19]. However, conceptually, under HF concept, the document combines the entire cardiovascular continuum from risk factors for HF and initial signs of structural and functional myocardial remodeling (stages A and B) to clinically apparent and terminal disease stages (stages C and D) [19]. Such staging suggests the need to develop a differentiated approach to the global assessment of morbidity and mortality in HF, with the possibility of categorizing all HF patients into groups depending on phenotype, stage and management tactics. Their study at the level of Russian subjects and certain districts can make it possible to optimally plan material, technical and human resources. The presented study established significant differences in clinical and demographic characteristics, the burden on healthcare system, and mortality in groups identified by different codes. It can be assumed that the presence of I50.x code helps to identify patients with established symptomatic HF, characterized by common hospitalizations and high risk of adverse events. Indeed, mortality in the standard coding group was 15,7% compared with a mortality of 6,8% and 2,1% in the general and extended coding groups, respectively. The resulting differences in mortality may also be associated with a high prevalence of factors associated with poor prognosis, such as age, comorbidities, and hospitalizations. However, the method of data collection did not allow for multivariate analysis, taking into account all potentially influencing factors. At the same time, a recent meta-analysis demonstrated a one-year survival of patients with HF at the level of 86,5%, with significant heterogeneity between studies and patient groups [20]. Similar data on differences in survival for different HF phenotypes were obtained in The European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT-R), where among patients with acute HF, annual mortality was 23,6%, and among chronic HF patients — 6,4% [21]. It is important to emphasize that in routine domestic practice, all-cause mortality in patients after acute decompensated HF is 14,4%. However, with comprehensive specialized medical care and proper management with regular patient visits and telephone contacts, this indicator can be reduced to 4,1% [22].
We have demonstrated a high burden of HF on health care system — 4,2% of all medical encounters were made by HF patients, with every fifteenth hospitalization and every tenth emergency call for a HF patient. The high need for healthcare with frequent visits determines the cost of HF at the level of 1-2% of health care system [23]. The highest costs (up to 80%) are for HF hospitalizations with a high average bed day worth and frequent readmissions [23][24]. Over the past years, the number of hospitalizations with HF has been steadily increasing [25]. The United States study showed that HF was one of the top three causes of hospitalizations, accounting for 3,2% of all cases in 2018 [26]. In the study with 1077 HF patients, 83,1% of patients were hospitalized at least once during 4,7-year follow-up [27]. We found that 57% of patients were hospitalized at least once during the year. From the standpoint of healthcare organization, this emphasizes the need to improve the medical care system [28][29]. An extended HF coding approach may designate a subgroup of outpatients with a high need for preventive measures and control of cardiovascular risk factors to prevent overt HF, its further progression, and decrease the risk of adverse outcomes. Standard coding approach may designate a subgroup of very-high-risk patients with HF who require the development of a routing scheme, ensuring continuity and optimal therapy for HF, managing by a multidisciplinary team and organizing a home nursing.
Study limitations. Given that the study was performed in certain regions, results may not be representative of entire Russian population due to a possible selection bias. Differences between groups may be due not to the true characteristics of the contingent, but to coding peculiarities in hospitals or outpatient facilities. Clarification of the sensitivity and specificity of approach to assessing the HF prevalence and outcomes according to coding data in Russia may be the subject of further validation studies and quality audit. Improving the data collection system and recording all cases in the future in regional integrated database may affect the results, but at the moment one can assume a random probability of missing information from the database.
Conclusion
The prevalence of HF among the adult population of Saint. Petersburg in 2019 was 1,4%. HF was characterized by a high health care utilization and mortality rate reaching 15,7% per year. The use of different approaches to coding presumably could help to identify different groups of patients with HF, which requires the adaptation of healthcare models and an active monitoring system to reduce the risk of adverse events.
Relationships and Activities: none.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Soloveva A.E., Endubaeva G.V., Avdonina N.G., Kogan E.I., Gorbacheva T.V., Lubkovsky A.V., Yazenok A.N., Yakovlev A.N., Zvartau N.E., Villevalde S.V., Shlyakhto E.V. ICD-10 code-based definition of heart failure in Saint Petersburg electronic health records: prevalence, health care utilization and outcomes. Russian Journal of Cardiology. 2021;26(3S):4621. https://doi.org/10.15829/1560-4071-2021-4621
Copy