Types of hemodynamic response to orthostasis according to continuous blood pressure monitoring: a case series of heart failure with reduced ejection fraction
Heart failure (HF) is characterized by heterogeneous pathophysiological mechanisms of development and progression, a wide range of comorbidities, and is associated with a high risk of adverse outcomes [1][2]. To develop a personalized strategy for HF treatment, an extended examination and phenotyping is required [3-5]. An important tool for assessing hemodynamic stability in HF can be an active standing test (AST). The hemodynamic response in AST is an integral indicator and reflects the balance between factors of resistance to orthostatic hypotension (OH) (neurohumoral activation and systemic congestion) and factors that increase the risk of poor postural control, which accumulate as HF progresses. This can be used to stratify patients depending on the risk of adverse outcomes [6].
AST reflects the short-term response of cardiovascular and autonomic nervous system to body position changes [7]. According to the clinical guidelines for hypertension in adults [8], blood pressure (BP) measurement when moving from a sitting to a standing position is recommended for all patients at the first visit to detect OH, and for the elderly, patients with diabetes and other predisposing factors — at each subsequent visit. AST during the transition from lying to standing position is also included in the initial examination of patients with syncope [9] and is recommended for screening for OH in patients older than 65 years [10].
AST using a standard BP monitor is a simple and available screening method that allows identifying significant hemodynamic abnormalities. However, it only fragmentarily reflects the hemodynamic response in certain time intervals and does not allow assessing the baroreceptor reflex and key changes occurring during the first minute of orthostasis. AST with continuous beatto-beat BP monitoring represents the most complete characteristic of the hemodynamic response to orthostatic stress. According to the Consensus statement of the European Federation of Autonomic Societies endorsed by the American Autonomic Society and the European Academy of Neurology (2021) [7], AST with continuous beatto-beat BP monitoring, like tilt testing, should be performed for suspected reflex syncope (all forms), OH (all forms), and psychogenic pseudosyncope. To detect early OH, the continuous BP recording is necessary [9][11]. In addition, according to the analysis of the Atherosclerosis Risk In Communities (ARIC) study [12], which included 11429 participants (women, 54%; mean age, 54±5,7 years, AST with BP measurement during 2 min of orthostatic stress), OH identified precisely 1 minute after transition from prone to standing had predictive value for the risk of falls, fractures, syncope, and mortality, while no clear associations with long-term outcomes were obtained for measurements after the first minute.
Of particular interest is the study of AST results in patients with HF. HF has been considered one of the causes of secondary OH for many years [13]. A wide range of factors involved in the mechanisms of hemodynamics regulation in orthostatic stress in HF suggests the possibility of different responses to AST in this population [14]. However, there are few studies on the features of the orthostatic response in HF [14][15].
The purpose of presented case series was to show types of hemodynamic response in AST with continuous BP monitoring in patients with HF with reduced left ventricular ejection fraction (LVEF), as well as the available literature data on their clinical and prognostic role.
Material and methods
The presented data are part of the study of orthostatic reactions in HF patients, performed on the basis of the Almazov National Medical Research Center. The study protocol was approved by the Ethics Committee. All patients signed an informed consent.
The study included outpatients with documented HF with LVEF <40% receiving HF therapy according to clinical guidelines. All patients underwent standard diagnostic investigations, as well as cardiopulmonary testing.
AST was performed in the morning (until 12 a.m.). On the day of examination, participants took all prescribed medications except for a loop diuretic.
Procedure of active standing test. We performed continuous non-invasive BP and heart rate (HR) measurement using a “Kardiotekhnika-SAKR” system (Incart) on the right arm and by the standard auscultatory method based on the Korotkoff sounds using a microphone on the left arm. The right arm was fixed at chest level with a elbow brace. During the entire test, a 12-lead electrocardiography was performed in parallel.
AST included following elements:
1) 10-minute stay in ф prone position, during which continuous BP recording on the right arm and four-fold BP measurement on the left arm (at 4, 6, 7 and 9 minutes) were performed;
2) Transition to vertical position on command with prior notice and a countdown from 5 to 1;
3) A 5-minute stay in a standing position, during which continuous BP recording on the right arm and three-fold BP measurement on the left arm (1, 3 and 5 minutes) were performed.
The total AST duration was 15 minutes.
Determining types of hemodynamic response. The classification and criteria of hemodynamic response types in AST with continuous BP monitoring proposed in the consensus statement [7] (Table 1) were used. Since the definition of orthostatic hypertension (OHT) is not unified, the most commonly used criterion for increased systolic blood pressure (SBP) ?20 mmHg was used [16].
Table 1
Classification of pathological types of hemodynamic response in orthostatic stress

Abbreviations: BP — blood pressure, DBP — diastolic blood pressure, OH — orthostatic hypotension, POTS — postural orthostatic tachycardia syndrome, SBP — systolic blood pressure, HR — heart rate.
Results
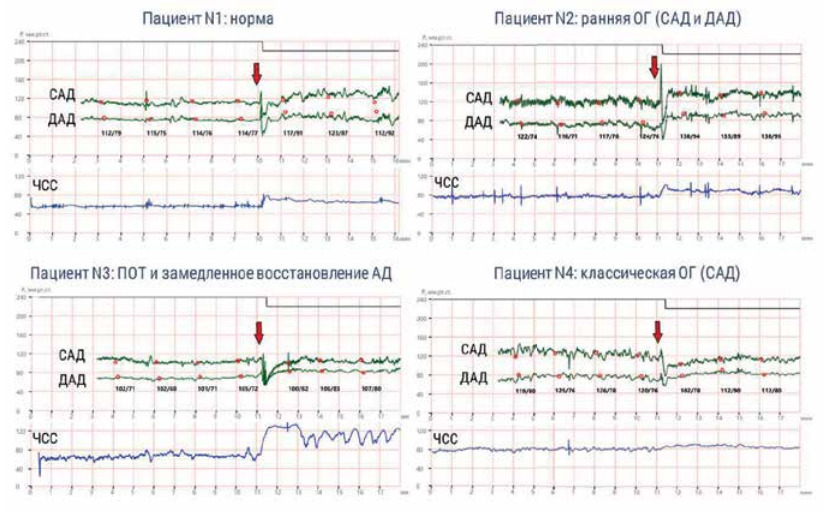
These case series included data from 4 patients with dilated cardiomyopathy without prior myocardial infarction, coronary revascularization, diabetes, chronic kidney disease, cancer and other significant diseases. All patients had sinus rhythm at the time of AST. Main characteristics are presented in Table 2. Trajectories of BP and HR, identified during AST with continuous BP monitoring, are shown in Figure 1.

Figure 1. Types of hemodynamic response in orthostatic stress in patients HF with reduced EF.
Note: the figure shows SBP and DBP values obtained by standard BP measurement (red dots) (four times in the supine position and for 1, 3 and 5 minutes upon standing). The arrow indicates the moment of transition from the supine to standing position. Green lines — continuous BP monitoring, blue line — continuous HR monitoring.
Abbreviations: BP — blood pressure, DBP — diastolic blood pressure, OH — orthostatic hypotension, OHT — orthostatic hypertension, POTS — postural orthostatic tachycardia syndrome, SBP — systolic blood pressure, HF — heart failure, HR — heart rate.
Table 2
Clinical, demographic and paraclinical characteristics of patients

Notes: * — all significant cardiovascular pathologies and comorbidities are listed, ** — all patients had no crackles on lung auscultation,
*** — drug therapy included:
Patient N1: valsartan+sacubitril 150 mg 2 times a day, bisoprolol 12,5 mg, spironolactone 12,5 mg, torasemide 2,5 mg, amiodarone 200 mg;
Patient N2: valsartan+sacubitril 100 mg 2 times a day, bisoprolol 5 mg, torasemide 5 mg, warfarin 5 mg, acetylsalicylic acid 100 mg, atorvastatin 20 mg;
Patient N3: valsartan+sacubitril 100 mg 2 times a day, bisoprolol 1,25 mg, torasemide 2,5 mg, acetylsalicylic acid 75 mg;
Patient N4: valsartan+sacubitril 50 mg 2 times a day, metoprolol succinate 75 mg, spironolactone 25 mg, torasemide 2,5 mg, acetylsalicylic acid 75 mg, rosuvastatin 40 mg.
Abbreviations: MRA — mineralocorticoid receptor antagonists, ARNi — angiotensin receptor-neprilysin inhibitors, DBP — diastolic blood pressure, F — female, ICD — implantable cardioverter-defibrillator, BMI — body mass index, M — male IVC — inferior vena cava, RV — right ventricle, SBP — systolic blood pressure, LVEF — left ventricular ejection fraction, HR — heart rate, NYHA — New York Heart Association, TAPSE — tricuspid annular plane systolic excursion, VO2/kg — peak oxygen consumption at cardiopulmonary testing.
In a relatively homogeneous group of patients with HF with reduced LVEF, various variants of hemodynamic response were demonstrated during AST. Patient N1 had a normal response, patient N2 — initial OH, patient N3 — postural orthostatic tachycardia syndrome (POTS) accompanied by delayed BP recovery, and patient N4 — classic OH. With standard BP measurement on the arm in patient N4, the criteria for classical OH were met for 1 min of orthostatic stress (decrease in SBP by 22 mm Hg), but not for 3 minutes (decrease in SBP by 12 mm Hg); patients N1, N2 and N3 had a normal BP response.
Clinical symptoms during AST were present only in patient N3 and were manifested by dizziness lasting ~20 sec, which occurred immediately after the transition to a standing position, but did not require testing termination.
Discussion
This paper presents a heterogeneous profile of hemodynamic response during AST with continuous BP recording in a relatively homogeneous group of stable, predominantly middle-aged patients with dilated cardiomyopathy, reduced LVEF and preserved right ventricular function, receiving similar therapy (angiotensin receptor-neprilysin inhibitors, beta-blockers and loop diuretics) and do not have significant comorbidities associated with the risk of orthostatic intolerance (OI). Three of the four cases were asymptomatic during AST, and only one patient prior syncope. At the same time, prior IO symptoms were absent only in a patient with a physiological response in orthostatic stress. It is important to emphasize that if AST was performed with standard BP measurements, initial OH and delayed BP recovery would not have been detected. In addition, the classic OH in patient N4 might have been underestimated because the difference between standing and lying SBP met the OH criteria during the first but not the second BP measurement. It should be noted that the POTS prevalence in HF patients may remain underestimated, since betablocker dose titration is needed. The presence of POTS in a patient N3 may be due to an insufficient dose of bisoprolol.
Normally, the transition to standing is accompanied by an intravascular blood redistribution from the chest to the abdominal cavity and lower limb vessels, which leads to a transient BP decrease by 4-5 mm Hg. In response to this, baroreflex activation, sympathetic nervous system stimulation, as well as a decrease in parasympathetic nervous system activity occurs, and, as a result, a compensatory shortterm increase in HR and vasoconstriction, which allows stabilizing the BP level [14]. If the regulatory mechanisms are impaired at any level, OH occurs — a pathological hemodynamic response in orthostatic stress with or without clinical manifestations (symptoms, falls and syncope) [7][9].
The most complete picture of hemodynamics in orthostatic stress is given by continuous noninvasive BP measurement. The method is based on a continuous assessment of the volume of finger vessels by a photoplethysmographic signal and electro-pneumatic system that creates pressure that counteracts a change in artery diameter under the cuff. BP and HR monitoring in each cardiac cycle allows to evaluate the hemodynamic response in real time throughout the entire orthostatic test, including immediately at the moment of transition to a standing position. Thus, it ensures a comprehensive assessment of trends, variability in BP and HR, baroreflex function, indirect determination of stroke volume and peripheral vascular resistance. In addition, AST with continuous BP monitoring can be combined with other methods: for example, with standard BP measurement on the other arm, parallel ECG recording, and conducting provocative tests [17]. The main advantages and disadvantages of continuous and standard BP recording are summarized in Table 3.
Table 3
Comparative characteristics of continuous BP monitoring with the standard BP measurement method

Abbreviations: BP — blood pressure, OH — orthostatic hypotension, OHT — orthostatic hypertension, POT — postural orthostatic tachycardia syndrome, PVR — peripheral vascular resistance, HR — heart rate, SV — stroke volume.
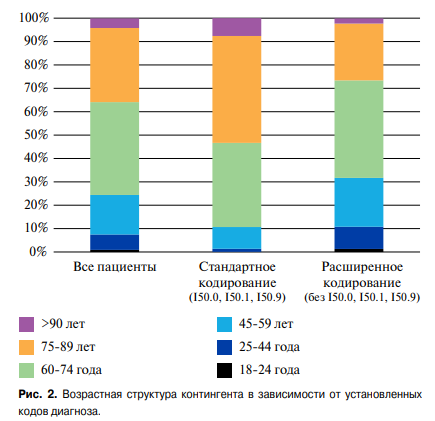
AST with 3-minute continuous BP monitoring may reveal following pathological types of hemodynamic response: initial OH, characterized by an excessive BP decrease upon standing, but adequate in terms of time and level of recovery; delayed orthostatic BP recovery, characterized by prolonged recovery time after standing, and classical OH, determined by a sustained BP. In addition, a sustained increase in HR upon standing can be recorded — POTS (Figure 2).

Figure 2. Types of the hemodynamic response with continuous BP monitoring in AST.
Note: no transient HR increase upon standing may indicate the presence of neurogenic autonomic dysfunction.
Abbreviations: BP — blood pressure, DBP — diastolic blood pressure, SBP — systolic blood pressure, HR — heart rate.
The pathophysiological mechanisms underlying different types of response are interrelated, but at the same time have their own characteristics. Initial OH is associated with a mismatch between cardiac output and systemic vascular resistance [18]. At the same time, it is a typical pathological response in AST (unlike the tilt testing), and thus the rapid BP recovery is probably associated with effective contraction of lower limb and abdominal muscles [19]. In turn, the delayed orthostatic BP recovery is presumably caused by baroreflex dysfunction, manifested by a decrease in vasoconstriction function. This confirms the fact that delayed BP recovery is observed after surgical carotid sinus denervation, and is rare in natural aging. Importantly, vasoconstrictioninhibited drugs (eg, alpha-blockers) also contribute to delayed BP recovery, which may be important in HF patients [18].
Classical OH, depending on the duration, can be transient and sustained. In HF, transient OH is due to drug therapy — hypovolemia caused by diuretic drugs, vasodilation and chronotropic incompetence caused by beta-blockers, digoxin and antiarrhythmic agents. At the same time, the combination of several drugs capable of inducing OH may increase its risk; however, data on these associations are limited. On the contrary, a meta-analysis of randomized clinical trials of various antihypertensive regimens, including individual data from hypertensive patients, showed a decrease in OH risk with more intensive BP control [20]. In turn, sustained OH in HF can occur in the presence of a morphofunctional substrate affecting the pathogenetic links of OH. Thus, impaired systolic function may result in an inability to provide adequate cardiac output during redistribution of blood flow and is most often discussed as the main cause of OH in HF. In addition, common HF comorbidities such as anemia, diabetes, chronic kidney disease, thyroid dysfunction, alcohol abuse, and lower limb skeletal muscle weakness also contribute to the OH development [13]. However, the key pathophysiological mechanism linking HF and OH, which is based on both OH and OHT, is autonomic dysfunction [14]. HF is seen as a state of autonomic dysfunction and thus may represent a secondary cause of sustained OH.
Currently, data on the clinical and prognostic significance of individual hemodynamic variants of OI are limited and do not answer about the causes of their development and related outcomes. The existing information on the features of hemodynamic response in orthostatic stress with continuous BP measurement was obtained mainly from The Irish Longitudinal Study on Ageing (TILDA) study, which did not include HF patients. It has been shown that initial OH is a common cause of unexplained syncope (7-14%), but is less significant without clinical symptoms and is not associated with poor prognosis. At the same time, delayed BP recovery is associated with cognitive decline, falls, fractures, and mortality [21]. It should be noted that hemodynamic deviations in BP and HR, assessed by the method of continuous BP recording, occur both in the form of individual OI phenotypes (like classic OH in patient N4), and in combination. Delayed BP recovery in 60% of cases is accompanied by initial OH [18]. In the Malaysian Elders Longitudinal Research (MELoR) study with an Asian population of elderly patients (n=1245; mean age, 67 years) [22], the combination of classic and initial OH was observed in 50% of cases, while single initial OH occurred in 13% , and classic — in 12% of cases. In the TILDA study, combinations of abnormal hemodynamic response types in AST with continuous BP monitoring in elderly patients without HF were predictors of OI and falls [23]. In the single-center study, SBP at 3-5 min of standing was an independent predictor of death and hospitalization in HF patients [6]. However, in general, the problem of OI in HF patients remains poorly understood. AST is not presented in either Russian or foreign clinical guidelines for HF [3-5]. To answer the question about the types of orthostatic responses, their prevalence and associations in Russian population, a multicenter prospective observational GRAVITY-HF study [15] was initiated, which uses a standard AST in patients with stable and decompensated HF. Continuous BP monitoring in the population of HF patients requires further study.
Conclusion
In the presented study, using the example of 4 cases of HF with reduced ejection fraction, various types of the hemodynamic response in AST with continuous BP recording were demonstrated: initial OH, delayed BP recovery, classic OH and POTS. Initial OH and delayed BP recovery can only be detected with continuous BP recording. Therefore, this method can be an important tool in the examination of HF patients, allowing identifying pathological response patterns within the first minute, which is the most important from a prognostic point of view.
The presented case series illustrate various types of the hemodynamic response and do not reflect its true prevalence in HF patients. The limited availability of continuous BP monitoring does not allow estimation of the true prevalence of hemodynamic response types in the general population of HF patients. In addition, data on their reproducibility, regardless of orthostatic test technique, are insufficient and contradictory [24] and require further study.
Relationships and Activities: none.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Fedorova D.N., Solovieva A.E., Galenko V.L., Kozlenok A.V., Berezina A.V., Villevalde S.V. Types of hemodynamic response to orthostasis according to continuous blood pressure monitoring: a case series of heart failure with reduced ejection fraction. Russian Journal of Cardiology. 2021;26(3S):4574. https://doi.org/10.15829/1560-4071-2021-4574
Copy