Thrombolysis versus unfractionated heparin for hemodynamically stable patients with pulmonary embolism: a systematic review and meta-analysis
Аннотация
Currently, thrombolytic therapy (TLT) for pulmonary embolism (PE) is recommended only for patients with high-risk PE. At the same time, in real practice, TLT is often performed in hemodynamically stable patients. The main contradiction arises due to the different risk-benefit ratio of TLT in comparison with anticoagulant monotherapy.
Aim. To assess the benefits of TLT, compared with unfractionated heparin (UFH) monotherapy, in hemodynamically stable patients with PE in reducing mortality, recurrence of PE and risk of bleeding.
Material and methods. Randomized controlled trials were searched in PubMed, Embase, and Cochrane Library databases. Of the 3050 publications found, 100 papers were selected for a detailed study. As a result of detailed analysis, 7 randomized clinical trials (n=1611) remained according to established criteria.
Results. TLT in hemodynamically stable patients with PE, in comparison with UFH, showed a tendency to decrease in the inhospital death rate: 2,39% vs 3,68 (odds ratio (OR): 0,73; 95% confidence interval (СI): 0,34-1,57), and a decrease in the composite endpoint (death and/or recurrent PE): 3,14% vs 5,15% (OR: 0,61; CI: 0,37-1,01). There was a significant increase in the number of major bleeding: 8,81% vs 2,70% (OR: 3,35; 95% CI: 2,06-5,45). TLT in hemodynamically stable patients with PE to a greater extent can reduce the pulmonary blood pressure, perfusion defects according to lung scintigraphy, as well as the need for therapy intensification. However, the heterogeneity of studies and the small number of participants require caution when interpreting their results.
Conclusion. TLT in patients with PE and stable hemodynamics tends to reduce mortality and/or recurrence of PE, but increases the incidence of major bleeding. Further studies need to determine the phenotypes of hemodynamically stable patients with PE who would benefit from TLT.
Currently, thrombolytic therapy (TLT) for pulmonary embolism (PE) is recommended only for patients with high-risk PE (evidence level IA), because hospital lethality in this category of patients may exceed 40% [1]. The reasonability of TLT in patients with PE and stable hemodynamics at hospitalization has been discussed over the past three decades. The patients of this group have a significantly less risk of intrahospital death [2]. The main contradiction is in the different ratios of risk and benefit of thrombolysis in comparison with anticoagulant monotherapy in randomized controlled trials (RCTs) [1].
The meta-analysis is aimed to evaluate the benefits associated with TLT in the decrease in lethality, recurrent PE and the risk of bleeding compared with anticoagulant monotherapy in hemodynamically stable patients with PE.
Material and methods
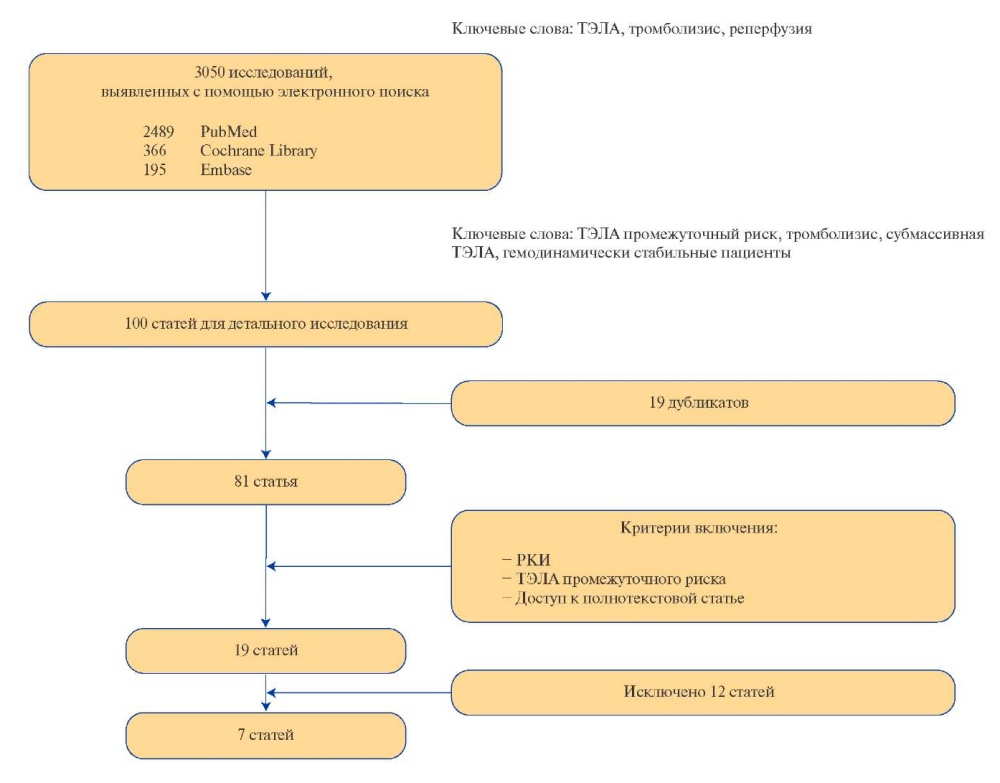
Search for publications and selection of studies. At first stage of the work, we performed the search for relevant sources in several electronic databases including PubMed, Embase, Cochrane Library for the period from 01.01.1970 to 31.12.2021 (last message). The search terms were — thrombolysis, thrombolytic therapy, pulmonary embolism, reperfusion, intermediate risk PE, hemodynamically stable РЕ, submassive PE. The language of publications is English. The information retrieval algorithm was developed in accordance with the reporting requirements and regulations for systematic reviews and meta-analyses (PRISMA) [3]. Abstracts of reports, protocols of meetings, monographs, clinical cases and series of cases were not included in the analysis. The selection process of the studies is shown in Figure 1.

Figure 1. The selection process of the studies included in the meta-analysis.
Abbreviations: RCT — randomized controlled trial, PE — pulmonary embolism.
Criteria for inclusion/exclusion. We included the RCTs that met the following criteria in the analysis: а) PE with stable hemodynamics/intermediate risk at hospitalization; b) the conduction of systemic thrombolysis; c) the use of unfractionated heparin (UFH) as a comparison anticoagulant; d) 18 years of age and older.
Initially, while selecting using the search queries described above, we obtained 2489 publications by PubMed, 366 publications — Сochrane Library, 195 publications from Embase.
The studies with participation of patients having high-risk PE/hemodynamically unstable, those concerning the catheter methods of administering thrombolytic agents, or comparing two different thrombolytic agents, or evaluating the different doses of the same drug, or about the use of low molecular weight heparins were excluded from the analysis.
From 3050 found publications, 100 articles were selected for a detailed analysis. It should be emphasized that the number of the patients included in the studies was not a determining factor of the selection. The access to the full-text version of the article was also necessary.
After analyzing the headings and their annotations, we found 81 articles that met the goal; then 19 repetitive publications were excluded. After evaluating full-text copies, we took 19 publications dedicated to RCTs about the use of systemic TLT for PE to analyze. Further, 8 publications included patents with high-risk PE [4-11], two studies about the use of 50% of TLT dose [12][13], one study about the use of low molecular weight heparins as an anticoagulant [14], and one study concerning the comparison of different methods of administering thrombolytic drug [15] were excluded from them. Finally, 7 publications met to primarily established criteria were left for analysis.
Data collection and analysis. To assess the risk of systematic errors in RCTs, we used an adapted and validated questionnaire in our work [16]. The risk of systematic errors was assessed as low (1 score), high (2 scores) and indefinite (0 scores). We assessed the effectiveness and safety of the intervention (TLT versus UFH therapy), using the odds ratio (OR) with 95% confidence interval (CI). The calculations were based on the random effects models at I2 >40%, P<0,10 and on the fixed effects model at I2 ?40%, Р?0,10. The main endpoints we interested were death during hospitalization period, major bleeding and composite endpoint (death during hospitalization period from all causes and/or recurrent PE). The analysis was performed using Review Manager (RevMan) version 5.4.
Results
The main characteristics of RCTs met to the criteria of inclusion are shown in Table 1; the risk of bias of the studies included in the meta-analysis is given in Table 2.
Table 1
Characteristics of the studies included in the systematic review

Abbreviations: nd — no data, UFH — unfractioned heparin, RV — right ventricle, r-tPA — recombinant tissue plasminogen activator, PE — pulmonary embolism, echoCG — echocardiography
Table 2
Domains of occurrence of systematic errors

The last RCT performed in this group of patients is dated 2014, and the later RCTs included either a half dose of a thrombolytic drug [13], or low molecular weight heparins as a comparison anticoagulant [14], or analyzed catheter administration of thrombolytic drugs immediately into pulmonary artery [17-20].
The total number of patients included in our meta-analysis was 1611. The number of centers in RCTs varied from 3 to 76. In 4 studies, recombinant tissue plasminogen activator (r-tPA) was used as a thrombolytic drug, in 3 studies — tenecteplase. All RCTs excepting the study of Meyer G, et al. [21], included a small number of patients therefore, mortality was a part of the composite endpoint.
The meta-analysis showed that TLT in patients with PE and stable hemodynamics had a tendency to decrease the frequency of hospital lethality (Figure 2): 2,39% vs 3,68% (OR: 0,73; 95% CI: 0,34- 1,57) and to decrease the composite endpoint — death and/or recurrent PE (Figure 3): 3,14% vs 5,15% (OR: 0,61; CI: 0,37-1,01). At the same time, there was a statistically significant increase in the number of major bleeding events (Figure 4): 8,81% vs 2,70% (OR: 3,35; 95% CI: 2,06-5,45).

Figure 2. Hospital lethality.

Figure 3. Hospital lethality and/or PE recurrence.

Figure 4. Major bleeding events.
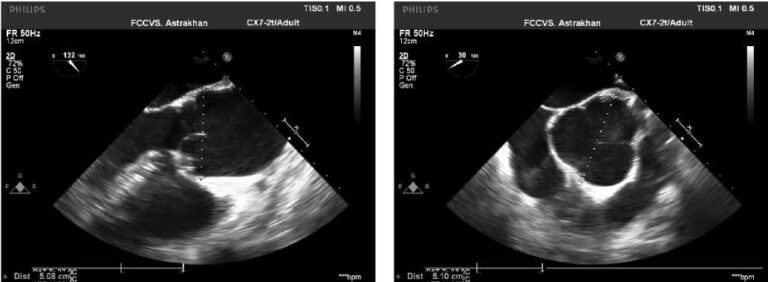
Previously, it was shown that the administration of a thrombolytic drug reduces pressure in the pulmonary artery (assessed by echocardiography [22-24] and angiopulmonography [25]), reduces the perfusion defects (assessed by lung scintigraphy [22] and angiopulmonography [25]) and reduces the need in therapy escalation [21][26] to a greater extent than UFH monotherapy. However, the heterogeneity of the studies and the small number of participants require to be cautious in interpreting the results of such publications.
For instance, in the study of Dalla-Volta С, et al. [25], the degree of pulmonary obstruction according to the Miller index, assessed by angiography of the pulmonary artery significantly decreased in the patients who received r-tPA from 28,3±2,9 mm Hg to 24,8±5,2 mm Hg (p<0,01), whereas in the UFH group there was no reliable dynamics. Mean pulmonary pressure decreased from 30,2±7,8 mm Hg to 21,4±6,7 mm Hg in the r-tPA group and even increased in the UFH group: from 22,3±10,5 to 24,8±11,2 mm Hg (p<0,01).
In the study of Goldhaber SZ, et al. [22], in the TLT group there was the improvement in the right ventricular (RV) wall excursion in 24 hours compared with the initial level in 39% of patients (16 patients), worsening — in 2% (1 patient). The same indicators in the UFH group were — 17% (8 patients) and 17% (8 patients), respectively (р=0,005). In patients who received r-tPA, a significant improvement in pulmonary perfusion was recorded. The volume of non-perfused lung areas decreased by 14,6% (from 42,9% to 28,3%) compared with the decrease by 1,5% in the group of patients who received UFH (from 36,0% to 34,5%, p<0,0001).
In the study of Konstantinides S, et al. [26], the frequency of the primary endpoint (hospital death or escalation of treatment) was significantly higher in the UFH plus placebo group than in the UFH plus alteplase (24,6% (34 patients) vs 11,0% (13 patients), р=0,006). The escalation of treatment meant the need for infusion of inotropic drugs due to persistent arterial hypotension or shock; repeated or “life-saving” thrombolysis; endotracheal intubation; cardiopulmonary resuscitation; and emergency surgical embolectomy or catheter thrombectomy. Probability of 30-day survival (according to KaplanMeyer analysis) was higher in the UFN+alteplase group (р=0,005). This difference was associated with a higher frequency of treatment escalation in the UFH+placebo group (24,6% vs 10,2%, р=0,004) because the hospital lethality was low in both groups (3,4% in the TLT group and 2,2% in the UFH+placebo group, р=0,71).
The study performed by Becattini C, et al. [23] showed that the decrease in the ratio of the enddiastolic volume of the right ventricle to the left ventricle in 24 hours in the TLT group was 0,31±0,08, while in the placebo group — 0,10±0,07 (p=0,04).
The study of Fasullo MD, et al. [24] showed that the use of TLT was accompanied by early decrease of the RV size (in 48 hours in the UFH group from 48±2,3 mm to 39±1,2 mm, in the TLT group — from 49±2,4 mm to 35±1,2 mm, р=0,0001; in 3 months in the UFH group — 27±1,3 mm, in the TLT group — 23±0,6 mm, р=0,001) and by a more favorable tendency in clinical outcomes. Also, in the TLT group, the decrease in systolic pulmonary artery pressure was more pronounced (from 57±18 mm to 38±7 mm in 48 hours and 12±3 mm in 6 months, р<0,001) than in the UFH group (from 58±19 mm to 47±11 mm in 48 hours and 18±2 in 6 months).
According to the data obtained by Meyer G, et al. [21], the hemodynamic disorders or acute heart failure occurred in 1,6% of patients while using TLT and in 5% in the UFH group (p=0,002).
The study of Klinе JA, et al. [27] reported about at least one adverse outcome: death, intubation, fatal intracranial hemorrhage in 37% of patients who received placebo+UFH and in 15% of patients who received TLT+UFH during 90 days of monitoring (р=0,017).
Discussion
The performed meta-analysis showed that the decrease in mortality and/or the frequency of PE recurrences by the use of TLT in patients with PE and stable hemodynamics is unreliable but the increase in frequency of bleeding events by the use of TLT is statistically significant. It should be especially noted that these data were obtained by the studies included a small number of patients, and the authors needed to create the composite endpoints to evaluate the benefit/risk of the interventions in both groups [22-27].
Actually, the only RCT that included >1 thousand intermediate-high risk patients with PE was Pulmonary Embolism Thrombolysis (PEITHO) [21]. In the PEITHO study, the benefits of TLT using tenecteplase (OR 0,44; 95% CI 0,23-0,87) were leveled by a significant increase in the number of major bleeding events (6,3% in the TLT group vs 1,5% in the group without TLT). This study was a landmark, after which in the recommendations of the European Society of Cardiology in 2019 [1] the place of reperfusion therapy in intermediate-risk PE was defined only as a “life-saving” procedure for patients with worsening hemodynamics against the background of anticoagulant therapy. The performed RCTs [22-25] confirmed the important role of TLT in the ability to reduce right ventricular dysfunction in intermediate-risk PE.
Clearly, TLT is not a method to treat all patients with intermediate-risk PE. And it is necessary to concentrate on finding predictors of hemodynamic worsening before the occurrence of obstructive shock in a patient, using the ability of TLT to quickly reduce the load on the right ventricle. Thus, the recommendations of the American College of Chest Physicians in 2021 [28] set out the position to begin the systemic TLT in patients with PE and an acceptable risk of bleeding, whose condition worsens after the start of anticoagulant therapy before the occurrence of shock or hypotension (weak recommendation, evidence with a low degree of reliability). It is suggested to conduct anticoagulant therapy to these patients, monitoring the signs of clinical worsening (decrease in systolic blood pressure, increase in heart rate, deterioration of gas exchange, the signs of insufficient perfusion, deterioration of RV function or increase in cardiac biomarkers).
The same conclusions were obtained in previously performed meta-analyses [29-34]. For instance, in 2009, Tardy B, et al. performed meta-analysis which included 5 RCTs [29] to compare the use of r-tPA vs UFH momotherapy in 464 hemodynamically stable patients with acute PE. The generalized assessment revealed statistically insignificant decrease in mortality associated with PE or recurrent PE while using r-tPA in comparison with UFH (3,5% vs 4,6%, p=0,73). Also, in the r-tPA group compared with UFH there was no significant increase in the number of major bleeding events (4,9% vs 4,6%, risk ratio (RR): 0,94; 95% CI: 0,39-2,27). The same results were obtained when taking only those studies that included the patients with echocardiographic signs of RV dysfunction. There was no decrease in either mortality due to PE, or the frequency of PE recurrences against the background of the administration of r-tAP compared with UFH in patients with stable hemodynamics.
In 2014, at once 4 meta-analyses to assess the effectiveness of TLT in the treatment of hemodynamically stable patients with PE were performed [30-33].
Chen H, et al. [30] included 15 RCTs in metaanalysis (totally 1247 patients), which compared UFN with various thrombolytic drugs (urokinase/ alteplase/tenecteplase). TLT was associated with significant decrease in the frequency of PE recurrences or death (1,94% vs 5,87%, OR: 0,37; 95% CI: 0,21- 0,66; without statistically significant heterogeneity between studies, P=0,49) with an unreliable increase in the number of major bleeding events (3,57% vs 2,67%, OR: 1,34; 95% CI: 0,70-2,58), but with significant increase of minor bleeding events (12,78% vs 3,65%, OR: 4,12; 95% CI: 2,37-7,17). However, unlike our study, that meta-analysis also included the studies with high-risk PE and 50% of dose of a thrombolytic drug.
Liu Y, et al. [31] compared r-tPA with UFH monotherapy (n=594 patients) in the meta-analysis based on 7 RCTs. The use of r-tPA was associated with insignificant decrease in mortality (2,75% vs 3,96%, р=0,520); PE recurrences (2,13% vs 3,34%, RR: 0,70; 95% CI: 0,28-1,73); insignificant (unreliable) increase in the number of major bleeding events (5,15% vs 4,29%, RR: 1,06; 95% CI: 0,520- 2,150). The same results were obtained when analyzing the subgroup of patients with echocardiographic signs of RV dysfunction. On the contrary, the use of r-tPA compared with UFH was associated with a significant decrease in the necessity of therapy escalation in the studies that also included the patients with the RV dysfunction (6,56% vs 19,7%; RR: 0,34; 95% CI: 0,20-0,65). The meta-analysis concluded that there is no data showing the advantage of r-tPA compared with UFH for the staring treatment of absolutely all hemodynamically stable patients with acute PE but r-tPA can be useful in the treatment of patients with RV dysfunction.
The meta-analysis performed by Marti К, et al. [32] (2057 patients, 15 RCTs) concluded that compared with UFH, TLT was associated with the reliable decrease in the total mortality (OR: 0,59; 95% CI: 0,36-0,96). However, this decrease turned out to be statistically insignificant after the exclusion of patients with high-risk PE from the pool of studies (OR: 0,64; 95% CI: 0,35-1,17). Thrombolysis was associated with a significant decrease in composite endpoint and/or therapy escalation (OR: 0,34, 95% CI: 0,22-0,53), with PE-related mortality (OR: 0,29; 95% CI: 0,14-0,60) and recurrent PE-related mortality (OR: 0,50; 95% CI: 0,27-0,94). Major bleeding (OR: 2,91; 95% CI: 1,95-4,36) and lethal or intracranial hemorrhage (OR: 3,18; 95% CI: 1,25- 8,11) were significantly more frequent in patients who received TLT.
The meta-analysis performed by Nakamura S, et al. [33] included 1510 patients. They did not obtain any significant differences in composite endpoint of death from all causes and/or PE recurrence between the TLT group and the group received only UFH (3,1% vs 5,4%; RR: 0,64; CI: 0,32-1,28). TLT has significantly decreased the frequency of the composite endpoint of death from all causes or clinical worsening (3,9% vs 9,4%; RR: 0,44; CI: 0,29-0,67). There were no statistically significant differences in the occurrence of major bleeding when comparing TLT with UFH monotherapy (6,6% vs 1,9%; RR: 0,44; 95% CI: 0,58-7,35). This meta-analysis also showed that reperfusion therapy does not significantly reduce the risk of mortality or PE recurrence in patients with acute submassive PE, but TLT prevents clinical worsening requiring escalation of treatment in patients with acute submassive PE. The assessment of bleeding risk can be the most successful approach for the improvement of clinical outcomes and patient-specific benefits of TLT.
The last, largest meta-analysis performed by Zuo Z, et al. [34] and published in 2021 included 21 studies, totally 2401 patients, among them the patients with massive PE and surgical interventions. The authors concluded that TLT may increase the risk of death from acute PE compared with UFH (OR: 0,58; 95% CI: 0,38-0,88); however, its efficiency was mainly caused by the studies performed in patients with high-risk PE. It is shown that TLT may be useful to reduce the risk of recurrent PE (OR: 0,54; 95% CI: 0,32-0,91) but it may cause major (OR: 2,84; 95% CI: 1,92-4,20) and minor bleeding events (OR: 2,97; 95% CI: 1,66-5,30) including hemorrhagic stroke (OR: 7,59; 95% CI: 1,38-41,72). In the article, the authors emphasize that these evidences are characterized by a low degree of reliability due to the high risk of bias of the RCTs included in the analysis.
Thus, nowadays, the TLT advantages in the decrease of hospital lethality and PE recurrences compared with the risk of bleeding in patients with high-risk PE have been proven, and this pattern is clearly visible even in the studies with a small number of patients [4-11]. In patients with PE and stable hemodynamics, not everything is so unambiguous. In our opinion, the use of TLT is justified in a narrow circle of patients with a low risk of bleeding and with criteria for the beginning hemodynamic deterioration for the purpose to timely unload the small circle of blood circulation, before the occurrence of obstructive shock. To confirm this hypothesis, it is advisable to conduct a planned RCT with a clear design and narrow inclusion criteria in patients with intermediate-high risk PE.
Limitations of the study. The present meta-analysis did not include the studies where low-molecularweight heparins or direct oral anticoagulants were used as anticoagulant therapy.
Conclusion
Our meta-analysis showed that TLT in patients with PE and stable hemodynamics tends to reduce mortality and/or the frequency of PE recurrences, but increases the frequency of major bleeding events. Systemic administration of thrombolytic drugs leads to faster lysis of thrombus than UFH monotherapy, thereby reducing pressure in the pulmonary artery, improving RV function and pulmonary hemodynamics. In further studies, it is necessary to determine the phenotypes of patients with PE and stable hemodynamics who will benefit from TLT.
Relationships and Activities: none.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Cherepanova N.A., Podlipaeva A.А., Andreeva E.S., Umyarova E.N., Mullova I.S., Pavlova T.V., Duplyakov D.V. Thrombolysis versus unfractionated heparin for hemodynamically stable patients with pulmonary embolism: a systematic review and meta-analysis. Russian Journal of Cardiology. 2022;27(3S):5120. https://doi.org/10.15829/1560-4071-2022-5120
Copy