Subanalysis of the AUGUSTUS trial
Atrial fibrillation (AF) is the most common type of cardiac arrhythmias, which, according to recent epidemiological studies, is recorded in 2-4% of the population [1]. In the coming decades, a further increase in the number of patients with AF is expected, both due to a general increase in life expectancy and a progress in diagnostics [2]. In recent years, a steady increase in the prevalence of diseases contributing to AF has been recorded — hypertension, coronary artery disease (CAD), diabetes, heart failure, chronic kidney disease, obesity [3][4][5]. As usual, when managing patients with AF, physicians are primarily concerned about such dangerous complications as cardioembolic stroke (due to hypercoagulation typical ofAF) or bleeding (due to the anticoagulation). However, according to statistics, cardiovascular causes of death are the most common — in 46% of cases, while death due to thromboembolism and bleeding — in 5,7% and 5,6%, respectively [6]. Indeed, nonvalvular AF and CAD are often observed in combination: up to 10% of patients requiring percutaneous coronary intervention (PCI) have AF [7]; the risk of new-onset AF associated with myocardial infarction (MI) is 60-77% [8]. AF occurs in 6-21% of patients with acute coronary syndrome (ACS), which unfavorably affects their prognosis due to an increased risk of ischemic stroke, as well as in-hospital and long-term mortality [9].
ACS and/or PCI in patients with AF requires the use of combined antithrombotic therapy (ATT). Until recently, this clinical setting required the considering administration of two antiplatelet agents (acetylsalicylic acid (ASA) and P2Y12 receptor blocker) and one oral anticoagulant (OAC) (triple ATT). However, such therapy increases the risk of bleeding 2-4 times [10][11], while the incidence of severe bleeding reaches 2,2% during the first month of treatment and 4-12% during the first year [12].
One of the first steps in solving the problem of high bleeding rate with triple ATT was the WOEST trial, which showed that dual therapy in these patients (vitamin K antagonist (VKA) warfarin and clopidogrel) significantly reduces the incidence of bleeding in comparison with triple therapy (warfarin, clopidogrel and ASA) [13]. At the same time, the incidence of any thrombotic events did not increase, and the 1-year all-cause mortality in the dual ATT group was lower than in triple ATT (2,5% and 6,4%, respectively; p=0,027).
The next step in optimizing management of patients with AF, ACS and/or PCI was the randomized clinical trials (RCTs) with direct oral anticoagulants (DOAC) — PIONEER AF PCI (riva- roxaban) [14], RE-DuAL PCI (dabigatran) [15] and AuguStuS (apixaban) [16]. These RCTs showed that DOAC in patients with AF, ACS and/or PCI significantly reduces the bleeding rate compared with warfarin, which confirmed the results of the WOEST trial.
The largest of these RCTs was the AUGUSTUS study, which evaluated the safety of apixaban versus VKA and aspirin versus placebo in patients with AF and/or ACS or PCI [16]. This study included 4,614 patients from 33 countries, including from Russia (n=762). It should be emphasized that the AUGUSTUS trial had a unique 2×2 factorial design, which made it possible to simultaneously evaluate two independent hypotheses:
- Comparison of apixaban at a dose of 5 mg twice a day and warfarin in combination with DAPT or P2Y12 receptor blocker in safety (International Society on Thrombosis and Haemostasis (ISTH) major or clinically relevant nonmajor bleeding).
- Comparison of P2Y12 blocker monotherapy and DAPT in safety (ISTH major or clinically relevant nonmajor bleeding).
In addition, the design of this study had several important differences from the PIONEER AF PCI and RE-DUAL PCI trials. First, a history of stroke or transient ischemic attack was not an exclusion criterion; second, the AUGUSTUS trial included patients with ACS and conservative management (23,9%); third, in patients who did not have standard indications for reducing apixaban dose, full dose was used — 5 mg twice a day. It is also important that randomization to aspirin/placebo took place within 14 days after ACS or PCI, and patients received ASA in an open-label manner for at least a week after the event. Thus, the design features of the AUGUSTUS trial provided evidence of the efficacy and safety of apixaban for actual clinical practice.
The primary endpoint (major and nonmajor clinically relevant bleeding) was recorded in 10,5% of patients in the apixaban group and 14,7% of patients in the warfarin group (hazard ratio (HR), 0,69; 95% confidence interval (Ci), 0,58-0,81; p<0,001). The frequency of bleeding in patients who received triple ATT with ASA was 16,1%, dual ATT — 9,0% (HR, 1,89; 95% CI, 1,59-2,24; p<0,001). Incidence of death or ischemic event (MI, stroke, stent thrombosis [definite or probable], or urgent revascularization) was comparable in the groups of patients receiving apixaban or warfarin (6,7 and 7,1%, respectively; HR, 0,93; 95% Cl, 0,75-1,16; p>0,05). This composite endpoint also showed a reduction in the stroke risk in the apixaban group versus the warfarin group — 1,2 and 2,4 per 100 patient-years (HR 0,50; 95% CI 0,26-0,97). The apixaban group compared with the warfarin one had a lower incidence of one of the secondary endpoints — death and hospitalization rates (23,5% vs 27,4%; HR, 0,83; 95% Cl, 0,74-0,93; p=0,002), which was achieved by reducing the number of hospitalizations.
Thus, the AUGUSTUS trial has shown that in patients with AF and indications for DAPT, apixa- banin combination with a P2Y12 receptor blocker is associated with a significant reduction of major and clinically significant nonmajor bleeding and hospitalization rate. In addition, the all-cause mortality and hospitalization rate was 17% lower with api- xaban compared with warfarin. The data from the AUGUSTUS trial supplemented the previous studies on apixaban, which showed its high safety profile compared to warfarin in patients with nonvalvular AF.
In general, the results of the PIONEER AF PCI, RE-DUAL PCI, and AUGUSTUS trials modified the use of combined ATT in AF patients who underwent ACS and/or PCI [17]. In the 2020 European Society of Cardiology (ESC) guidelines for AF [18], for the first time it is indicated that in AF patients with ACS undergoing an uncomplicated PCI, early cessation (<1 week) of aspirin and continuation of dual therapy with an OAC and a P2Y12 inhibitor (preferably clopidogrel) for up to 12 months is recommended if the risk of stent thrombosis is low or if concerns about bleeding risk prevail over concerns about risk of stent thrombosis, irrespective of the type of stent used (class — I, level of evidence — B). Triple therapy with aspirin, clopidogrel, and an OAC for longer than 1 week after an ACS should be considered when risk of stent thrombosis outweighs the bleeding risk, with the total duration (<1 month) decided according to assessment of these risks, and the treatment plan should be clearly specified at hospital discharge (class — IIa, level of evidence — C).
Triple ATT duration in patients with AF after PCI due to chronic coronary artery disease should be <1 week, after which ASA should be canceled. Continuation of dual therapy with OAC for up to 6 months and clopidogrel is recommended if the risk of stent thrombosis is low or if concerns about bleeding risk prevail over concerns about risk of stent thrombosis, irrespective of the type of stent used (class — I, level of evidence — B). Triple therapy with aspirin, clopidogrel, and an OAC for longer than 1 week should be considered when risk of stent thrombosis outweighs the bleeding risk, with the total duration (<1 month) decided according to assessment of these risks, and the treatment plan should be clearly specified at hospital discharge (class — IIa, level of evidence — C).
Given the need to use of a triple ATT for at least 1-4 weeks, it should be emphasized that among DOACs at the moment only apixaban has an evidence base on the efficacy and safety of use as part of a triple therapy in AF patients who underwent ACS and/or PCI, at the full dose registered for the prevention of stroke and systemic embolism. Other DOACs in this category of patients have been studied only as part of a dual therapy.
Above data suggests that the main complication, the risk of which necessitates the combined ATT, is stent thrombosis. This is the most dangerous complication of PCI, in which in-hospital mortality is 5-10%, and 30-day mortality is 10-25% [19][20][21].
The generally accepted ST classification was proposed in 2006 by the Academic Research Consortium (ARC) and adopted at the Food and Drug Administration (FDA) meeting [22]. Depending on the degree of diagnosis verification, the ARC classification subdivides ST into three categories:
Definite ST — angiographic or pathological confirmation:
- Angiographic confirmation of ST, based on an assessment of blood flow according to the Thrombolysis In Myocardial Infarction (TIMI) score, is considered sufficient if at least one of the following criteria is identified within 48 hours:
- Acute onset of ischemic symptoms at rest;
- New electrocardiographic changes suggestive of acute ischemia;
- Typical rise and fall in cardiac biomarkers (refer to definition of spontaneous myocardial infarction).
- Pathological confirmation of stent thrombosis (autopsy or examination of tissue retrieved following thrombectomy).
Probable ST — if the patient after PCI develops:
- Any unexplained death within the first 30 days after PCI.
- Regardless of the time after the index procedure, any myocardial infarction that is related to documented acute ischemia in the territory of the implanted stent without angiographic confirmation of ST and in the absence of any other obvious cause.
Possible ST — any unexplained death more than 30 days after PCI.
Effective prevention of ST, like any complication, is impossible without identifying the main risk factors. According to the 2020 ESC guidelines, the risk factors for ST in patients with coronary artery disease are stenting of left main stem or last remaining patent artery; suboptimal stent deployment; stent length >60 mm; diabetes mellitus; chronic kidney disease; bifurcation with two stents implanted; treatment of chronic total occlusion; and previous stent thrombosis on adequate antithrombotic therapy [18].
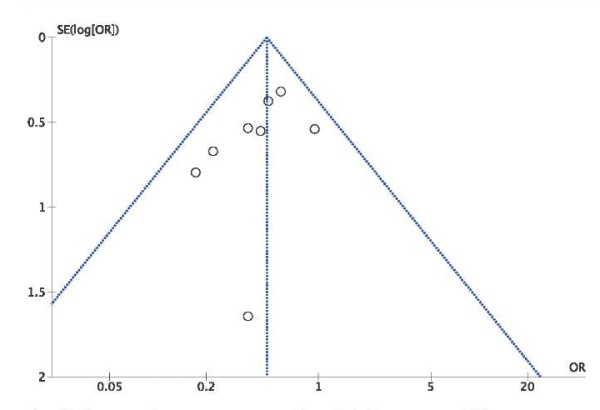
The results of the AUGUSTUS trial sub-analysis are extremely important, the purpose of which was to assess the frequency and timing of ST, as well as their outcomes in AF patients undergoing PCI [23]. Overall, this sub-analysis included 3,498 patients who underwent PCI. During the follow-up period (6 months), ST occurred in 57 (1,6%) patients. Of these, 20 (0,6%) cases were definite ST, 10 (0,3%) — probable and 27 (0,8%) – possible. Most of the events (80%) occurred within the first 30 days after PCI. Number of patients with definite or probable ST after 6 months was 13 (0,74%) for apixaban and 17 (0,97%) for warfarin (HR, 0,76; 95% Cl, 0,37-1,56); 11 (0,63%) for aspirin and 19 (1,08%) for placebo (HR, 0,58; 95% CI, 0,28-1,22). The incidence of ST in the groups of apixaban with aspirin, apixaban without aspirin, warfarin with aspirin, and warfarin without aspirin was 5 (0,57%), 8 (0,91%), 6 (0,69%), and 11 (1,26%), respectively.
Sub-analysis also showed an increase in the bleeding rate in the group of patients taking ASA, almost 2 times. In order to prevent one ST in the first month after PCI in the ASA group compared with the placebo group, 176 patients need to be treated, and to cause one serious bleeding — 100. The number of patients who need to be treated for 6 months to avoid one ST in the aspirin versus placebo group is 222, and 41 to cause one major bleeding.
Thus, among patients with AF and recent PCI who took aspirin for only the first week, ST is rare and the most events occur n the early period after PCI. The incidence of ST is lower with aspirin versus placebo, and with apixaban versus warfarin. The authors conclude that the results obtained justify the use of apixaban and the P2Y12 inhibitor without aspirin for the first 6 months for most patients, given the almost two-fold increase in bleeding with aspirin. In patients with a high risk of stent thrombosis and a low risk of bleeding, aspirin should be considered for 30 days after PCI.
Thus, the findings of the AUGUSTUS sub-analysis published in March 2020 [23] are fully consistent with the new ESC guidelines for the management of patients with AF and ACS and/or PCI [18].
European guidelines pay attention to the risk assessment of bleeding in patients with AF, for which it is advisable to use the HAS-BLED score. However, it must be remembered that over time the bleeding risk can vary significantly depending on the patient’s condition and concomitant therapy. That is why risk restratification should be carried out regularly, while high-bleeding-risk patients (HAS- BLED score >3) require more frequent reassessment [18]. This document also recommends that high-bleeding-risk patients should receive reduced dose of rivaroxaban (15 mg 1 time a day) and dabi- gatran (110 mg twice a day) (class — IIa, level of evidence — B). At the same time, apixaban in this category of patients should be used in full dose, given its favorable safety profile. ESC guidelines also noted the resumption of anticoagulation after a recent bleeding. The physician’s attention should be directed towards addressing the predisposing pathology (e.g. bleeding ulcer or polyp in a patient with gastrointestinal bleeding), and the reintroduction of OAC should be carried out as soon as feasible, as part of a multidisciplinary team decision. Consideration should be made for drugs such as apixaban 5 mg twice a day or dabigatran 110 mg twice a day, which are not associated with an excess of gastrointestinal bleeding compared with warfarin.
AUGUSTUS trial also indicated a lower incidence of one of the secondary endpoints (mortality and hospitalization rate) in the apixaban group compared with the warfarin group, which was achieved by reducing the number of hospitalizations. Subanalysis showed that during the study, a total of 1,125 patients (24,4%) were hospitalized, of which 384 (34,1%) had 2 or more hospitalizations [24]. Among the study participants, 780 patients (16,9%) were hospitalized at least once due to cardiovascular disease, 208 (4,5%) — due to bleeding, and 359 (7,8%) — due to another reason. At the same time, the frequency of hospitalizations was lower in the apixaban group compared with the warfarin group (22,5% vs 26,3%; HR, 0,83; 95% Cl, 0,74-0,93; p=0,002), which was explained by lower hospitalization rate for cardiovascular diseases (15,4% vs 18,5%;,HR, 0,81; 95% Cl, 0,71-0,94) and bleeding (3,6% vs 5,4%; HR 0,65; 95% CI, 0,50-0,86). Hospitalization rates did not differ between the aspirin and placebo groups (25,4% vs 23,4%; HR 1,10; 95% Cl, 0,98,1,24), as well as the hospitalization rate due to cardiovascular diseases (16,8% vs 17,0%; HR, 0,99; 95% Cl, 0,86-1,14). However, the hospitalization rate due to bleeding was more than 2-fold higher in patients receiving aspirin than placebo (6,1% vs 2,9%; HR, 2,11; 95% Cl, 1,58-2,81).
Of particular interest are the AUGUSTUS trial analysis concerning the conservative treatment of ACS, which consisted of 1097 patients. In fact, this analysis is the only large study that examined 6-month outcomes in patients with AF and ACS treated conservatively, since such patients were not included in the PIONEER AF PCI and RE-DUAL PCI studies. The number of major and nonmajor clinically relevant bleeding in case of conservative treatment was lower in apixaban group compared with warfarin in ACS (HR, 0,44; 95% Cl, 0,28-0,68; p=0,052) At the same time, the risk of death and hospitalization in this group of patients was significantly lower with apixaban compared with warfarin (HR, 0,71; 95% Cl, 0,54-0,92). Aspirin was more likely than placebo to cause bleeding in the conservative therapy group (HR, 1,49; 95% CI, 0,98-2,26; pinteraction=0,479), and the incidence of the composite endpomts ‘death/hospitalization’ and ‘death/ischemic events’ did not differ in the aspirin and placebo groups (pinteraction =0,787 and 0,710, respectively). As a result, thenbiaeecfing risk with apixaban was 56% lower than with VKA, and the risk of death or hospitalization was 29% lower with apixaban than with VKA. In contrast, the bleeding risk was 49% higher with aspirin compared with placebo, with no significant difference in mortality and ischemic events. Thus, the data obtained in patients with AF and ACS with conservative management support the combination of apixaban with a P2Y12 inhibitor, at least during the first 6 months
It should be emphasized once again that, in accordance with the AUGUSTUS trial design, the overwhelming majority of patients in the apixaban group received it at a full dose of 5 mg twice a day. At the same time, the safety profile of apixaban was significantly better than the warfarin. This pattern maintained in all subgroups of the study.
Conclusion
Comorbidity is typical of a modern patient. The combination of AF and various types of coronary artery disease is widespread in actual clinical practice, which worsens the patient’s prognosis. The management of AF patients who have undergone ACS and/or PCI is a challenging task that large- scale clinical trials help to solve. The AUGUSTUS trial confirmed that full-dose apixaban is superior in safety to warfarin, while not inferior in effectiveness. This pattern maintained in several significant sub-analyses devoted to such problems as stent thrombosis, hospitalization rate, and conservative management of patients with ACS. The findings of the AUGUSTUS trial are reflected in the 2020 ESC guidelines for the management of AF patients.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Pavlova T.V., Duplyakova P.D., Shkaeva O.V., Krivova S.P. Subanalysis of the AUGUSTUS trial. Russian Journal of Cardiology. 2020;25(3S):4104. https://doi.org/10.15829/1560-4071-2020-4104
Copy