Спонсорский материал
SIRENA score for in-hospital mortality risk assessment in patients with acute pulmonary embolism
Modern treatment of pulmonary embolism (PE) according to the European Society of Cardiology guidelines [1] involves risk stratification. The currently used risk stratification is based on clinical manifestations of the disease, echocardiographic data, assessment of myocardial necrosis markers, and also on the assessing combined risk using the pulmonary embolism severity index (PESI) or its simplified version (sPESI) [2]. At the same time, the practical use of the PESI or sPESI scores shows that some important factors, undoubtedly associated with the prognosis, remain outside this index, which can reduce the accuracy of risk stratification.
The aim was to create a new prognostic scale for in-hospital mortality risk assessment in patients with PE.
Material and methods
The study was based on the Russian register of acute pulmonary embolism SIRENA. The peculiarities of register organization, inclusion and exclusion criteria, as well as the main results are described in detail in previous publications [3]. Inclusion in the register was carried out sequentially for 12 months from April 2018 to April 2019 in 20 hospitals in 15 cities of Russia. The creation of a predictive scale was not the primary aim of the register and the analysis was performed retrospectively.
Statistical analysis. Independent predictors of in-hospital mortality became components of the novel prognostic score. The identification of these factors was carried out by univariate and multivariate regression analysis. Since the register protocol did not provide assessing the full PESI score, the predictive value of the new score was compared with the sPESI score. Comparison of prognostic scores was carried out by assessing the areas under the ROC curves.
Results
Characteristics of patients. The register included 609 patients (women — 50,7%, mean age — 63,0±14,5 years, minimum-maximum — 19-94 years). In the past, PE was in 56 (9,2%) patients, deep vein thrombosis — in 118 (19,4%) patients. During the 12 months preceding hospitalization, 95 patients (15,6%) underwent surgery, 77 (12,6%) had a long period of immobilization, 25 (4,1%) had limb fractures, 18 (3,0%) had myocardial infarction, 19 (3,1%) took oral contraceptives.
One hundred four patients (17,1%) had a history of cancer, of whom 36 (34,6%) had distant metastases, and 34 (32,7%) patients received treatment for an active cancer at the time of PE.
One hundred forty-two patients (23,3%) had a history of heart failure, 116 (19,0%) — atrial fibrillation, 400 (65,7%) — hypertension, 90 (15,2%) — diabetes, 55 (9,0%) — chronic kidney disease, 54 (8,9%) — chronic obstructive pulmonary disease.
When included in the register, the proportion of patients with systolic blood pressure (BP) <100 mm Hg was 11,8%, the proportion of patients with tachypnea (respiratory rate >30 bpm) — 2,8%, the proportion of patients with tachycardia (heart rate >110 bpm) — 17,7%, the proportion of patients with reduced oxygen saturation (SpO2 <90%) — 20,2%.
Cyanosis with PE signs was detected in 176 (30,2%) patients. Lower limb asymmetry and edema was observed in 217 (35,6%) and 223 (36,6%) patients, respectively.
Shortness of breath was the most common manifestation of PE. Five hundred forty (90,4%) patients complained about it. One hundred seventy- eight patients (29,8%) had chest pain as the main symptom, and 179 (30,0%) had syncope.
The sPESI score was assessed in 586 (96,2%) patients, while a low risk of death (sPESI score of 0) was found in 205 (33,7%) patients.
Thrombolytic therapy during hospitalization was carried out in 152 patients with PE (25,0%). Five hundred sixty patients (92,0%) received anticoagulant therapy in the hospital, while parenteral anticoagulants were used in 474 (77,8%) patients and oral anticoagulants — 457 (75,0%) patients.
During the hospitalization (media, 11 days; 1-3 quartiles, 7-15 days), 60 patients died. Mortality rate was 9,9%.
Creation of a predictive score. Univariate regression identified 52 factors associated with death during hospitalization, which were studied using multivariate regression. The results of this analysis identified independent predictors of in-hospital death (Table 1).
Table 1
Independent predictors of in-hospital mortality in patients included in the SIRENA register

Note: creatinine clearance calculated using the Cockcroft-Gault equation.
Abbreviations: CI — confidence interval, OR — odds ratio, PE — pulmonary embolism.
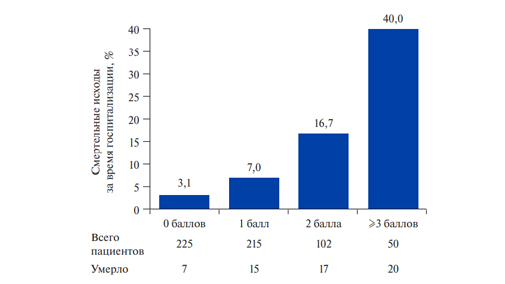
Subsequently, to create a prognostic score, it was decided to consider each of the independent predictors of death as one of the components of a novel score. It was decided to compare the accuracy of two possible models: the more complex (when each score component was assigned a value approximately equal to its odds ratio) and the simplified (when each score component was assigned a value of 1). Areas under the ROC curve values for a complex and simplified model did not differ significantly (Figure 1). Therefore, for practice it was advisable to use a simplified model (SIRENA score — Table 2).

Figure 1. Areas under the ROC curves for the simplified and complex versions of the SIRENA score.
Abbreviation: CI — confidence interval.
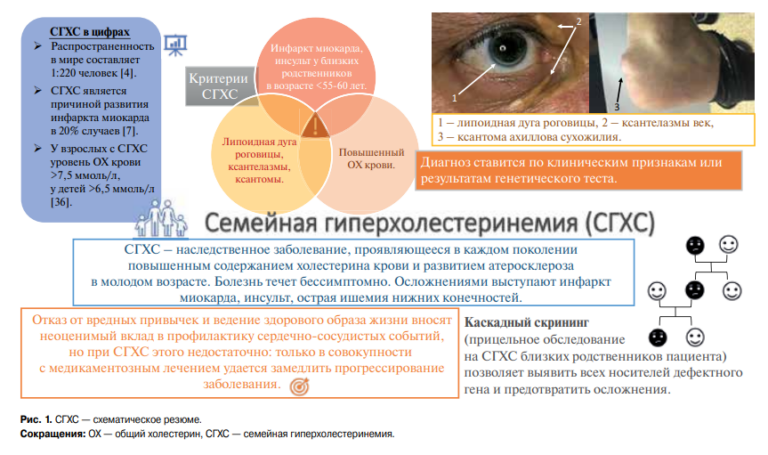
Predictive value of the SIRENA score. The relationship between various values of the SIRENA score and in-hospital mortality rate is shown in Figure 2, It can be seen that increased SIRENA score is associated with increased in-hospital mortality rate.

Figure 2. Relationship between different values of the SIRENA score and in-hospital mortality rate.
Due to the small number of patients with SIRENA score of 4 and 5, in Figure 2, data on patients with score ?3 are combined. At the same time, the difference between patients with 0 points and those with 1 point was insignificant (relative risk (RR), 2,24; 95% confidence interval (CI), 0,93-5,39), while between patients with 1 and 2 points and between patients with 2 and ? 3 points, the differences were significant (RR, 2,39; 95% CI, 1,24-4,59 and RR, 2,40; 95% CI, 1,38-4,16, respectively).
The ROC-curve value for the SIRENA score in relation to in-hospital mortality was 0,76 (95% CI, 0,69-0,83). The predictive sensitivity and specificity for high risk on the SIRENA score were 62,7% and 78,5%, respectively.
According to the ROC-curve, a cut-off point was found for dividing the SIRENA score into the low risk (0-1 points) and high risk ( ?2 points) categories for death during hospitalization. An almost five-fold significant difference in in-hospital mortality rate between high and low risk values on the SIRENA score was shown (RR, 4,87; 95% CI, 2,97-7,98; P<0,001 (Figure 3).

Figure 3. In-hospital mortality rate, depending on the high or low risk on the SIRENA score.
Abbreviations: CI — confidence interval, RR — relative risk.
Comparison of the predictive value of SIRENA and sPESI scores. In the study group, among 205 patients with low risk on the sPESI score (0), 7 people died during hospitalization (3,4%), and among 380 patients with high risk (?1), 53 people died (13,9%) (RR, 4,09; 95% CI, 1,89-8,82; p<0,001). The proportion of patients whose risks on the SIRENA and sPESI scores coincided (i.e., were either high or low on both scores) was 55,1%. The area under the ROC-curve for the sPESI score for in-hospital death was 0,73 (95% CI, 0,66-0,80). The difference with the similar parameter of the SIRENA score was insignificant (Figure 4).

Figure 4. Areas under the ROC curves for in-hospital mortality for the SIRENA and sPESI scores.
Abbreviation: CI — confidence interval.
In patients with high risk on both scores (sPESI+SIRENA), the mortality rate during hospitalization was 27,1%, which was significantly higher compared with patients at high risk only for sPESI — 13,9% (RR, 1,94; 95% CI, 1,36-2,82; p<0,001), but did not differ significantly in comparison with patients with high risk on the SIRENA score — 24,3% (RR, 1,11; 95% CI, 0,75-1, 65; p=0,78) (Figure 5).

Figure 5. In-hospital mortality rate in patients at high risk according to the sPESI, SIRENA score and their combination.
Abbreviations: CI — confidence interval, RR — relative risk.
Table 2
SIRENA* score
|
Factors |
Points |
|
Left ventricular ejection fraction <40% |
1 |
|
Immobilization in the previous 12 months |
1 |
|
Creatinine clearance <50 ml/min |
1 |
|
Syncope as a pulmonary embolism symptom |
1 |
|
Cyanosis on admission |
1 |
Note: * — total score is summed up.
Abbreviation: PE — pulmonary embolism.
Discussion
In the presented study, an attempt was made to create a new prognostic score to determine the risk of in-hospital mortality rate due to PE. The problem of predicting short-term outcomes in pulmonary embolism is quite relevant, since understanding the degree of risk is not only empirical knowledge, but also an important link in determining the management of patients.
Currently, the generally accepted prognostic model is the PESI and sPESI scores, which are the most accurate in comparison with other prognostic scores [2, 4-6]. At the same time, it is quite obvious that the sPESI score is not ideal and universal, since all possible factors of an unfavorable prognosis cannot be included in it (as in any other score). Therefore, the search for new opportunities to improve prognosis in patients with PE is of great clinical importance.
The data obtained in the SIRENA register is an important source of information on the management of patients with PE in Russian hospitals. But the prognostic score based on these results may become applicable not only in Russia, but also in other countries, since the main characteristics of the patients included in the SIRENA register were quite typical.
The novel prognostic score was created in the traditional way, by identifying independent predictors of deaths during hospitalization. It is interesting to note that most of the identified factors, on the one hand, can quite traditionally be associated with a poor prognosis in patients with cardiovascular diseases (reduced left ventricular ejection fraction, syncope, cyanosis, renal dysfunction). On the other hand, it should be noted that they do not directly coincide with risk factors in sPESI score (age, history of cancer or cardiopulmonary disease, low blood pressure, low blood oxygen level, tachycardia). The coincidences between some components of the
SIRENA and sPESI scores are only indirect (reduced blood oxygen level and cyanosis; cardiopulmonary disease and low left ventricular ejection fraction). This is probably why, in the studied group, the coincidence of death risk indicators between the scores was found only in 55% of patients, and the combination of high risk on both scores was associated with a significantly higher risk of death compared to patients who had a high risk on only one score.
An important prognostic component of the SIRENA score is syncope as a PE symptom. This is a well-known factor of poor prognosis, indirectly reflecting both the volume of the pulmonary artery lesion and right ventricular volume overload [7], as well as early in-hospital death [8]. In addition, syncope is an important diagnostic marker for PE. At the same time, such an obvious risk factor as low blood pressure was not selected in the SIRENA score. At first glance, this may seem like a disadvantage of the SIRENA score, but in fact it is advantage. After all, low blood pressure in PE is almost always an independent, separate factor of very high risk, and the presence of low blood pressure often does not require any other risk assessment. The fact that the blood pressure value is not taken into account in the SIRENA score gives it the potential to be more in demand in clinical practice.
In general, the combination of independent risk factors made up the SIRENA score even without using the numerical odds ratio values. Each of the score components has the same quantity, which is undoubtedly convenient for practical use. A specially conducted comparative analysis showed no advantages of a more complex score version.
The analysis of the predictive value of SIRENA score showed high sensitivity and specificity in predicting in-hospital mortality: 62,7% and 78,5%, respectively. At the same time, the area under the ROC-curve for the SIRENA score was quite high and practically coincided with this parameter in the sPESI score. Comparison of the SIRENA and sPESI scores showed that adding the SIRENA score to sPESI significantly increases the effectiveness of predicting a fatal outcome, while, on the contrary, adding the sPESI to the SIRENA score not increase its predictive accuracy. This may indicate a slightly greater practical value of the SIRENA score.
Study limitations. The creation of a predictive score was not the primary aim of the SIRENA register.
The assumption of a high predictive value of the novel score and its comparison with the sPESI should be validated with independent samples, preferably with a large number of patients.
Direct comparison of the SIRENA and sPESI scores may be limited, since the sPESI score was studied for 30-day outcomes, while the SIRENA score was studied for in-hospital events so far.
For further use of the SIRENA score, it is necessary to understand its predictive value for more distant outcomes (not just in-hospital outcomes), and in addition, determine the place of the score in decision-making on patient treatment.
Conclusion
Based on the Russian register of acute pulmonary embolism, the SIRENA score was developed, which has a high accuracy (sensitivity, 62,7%; specificity, 78,5%) in predicting in-hospital mortality.
The novel SIRENA score includes the following components: 1) left ventricular ejection fraction <40%; 2) immobilization in the previous 12 months; 3) creatinine clearance <50 ml/min; 4) syncope as a PE symptom; 5) cyanosis upon admission. The new SIRENA score is not inferior in predictive accuracy to the sPESI score recommended by the European Society of Cardiology guidelines, and the addition of the SIRENA score to the sPESI increases the predictive accuracy.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Erlikh A.D., Barbarash O.L., Berns S.A., Shmidt E.A., Duplyakov D.V. SIRENA score for in-hospital mortality risk assessment in patients with acute pulmonary embolism. Russian Journal of Cardiology. 2020;25:4231. https://doi.org/10.15829/1560-4071-2020-4231
Copy