Effectiveness of a comprehensive ambulatory monitoring system for patients with atrial fibrillation after cardioembolic stroke
Atrial fibrillation (AF) is a type of arrhythmia that occurs in 2-4% of the adult population. In the coming years, a further increase in AF prevalence is expected, both due to an increase in the life expectancy of population, and due to the improvement of diagnostic methods [1]. This arrhythmia is associated with a high risk of stroke and other thromboembolic events (TEE) [2][3]. Stroke is the leading cause of disability worldwide, and is also the second leading cause of death due to cardiovascular disease (CVD) [4]. According to modern statistics, the proportion of cardio-embolic stroke (CES) reaches 38% of all stroke ischemic events [5]. The pathogenesis of CES is based on occlusion of cerebral arteries by thrombi formed in the heart chambers, as a result of which, to reduce the risk of TEE, patients with AF should take oral anticoagulants for a long time [1][6].
After discharge from specialized neurological departments, patients with stroke are admitted to the outpatient stage of treatment. The tasks of this stage are to continue rehabilitation measures and carry out a set of preventive measures in order to prevent the repeated TEE and secondary complications of stroke. The success of stroke prevention in patients with AF depends on the appointment of optimal drug therapy by a physician and high medical adherence of a patient. However, despite the number of clinical guidelines regulating long-term therapy of patients with AF, there are currently no clearly developed programs for their outpatient management after a CES [7].
The aim of this study was to improve the longterm results of treatment of AF patients CES by creating and testing a comprehensive ambulatory monitoring system.
Material and methods
This study was performed in accordance with the Helsinki declaration and Good Clinical
Practice standards. The medical ethics committees of the Samara State Medical University approved this study. We included 139 patients with AF after CES for the period of 2016-2019 (women, 80 (57,55%); men, 59 (42,45%)). The mean age of the patients was 72,25±6,33 years.
The CES was confirmed in all patients by brain computed tomography (CT) or magnetic resonance imaging (MRI). AF has been documented by electrocardiography (ECG) or 24-hour ECG monitoring. Patients were treated in accordance with the current international guidelines for the management of patients with stroke and AF.
All patients underwent the following examination at the time of hospitalization:
- physical examination;
- laboratory diagnostics (complete blood count, biochemical blood test: albumin, urea, creatinine, lipid profile, glucose, alanine aminotransferase, aspartate aminotransferase, total bilirubin, potassium, sodium, coagulation testing, clinical urine test);
- instrumental tests (ECG, chest x-ray, echocardiography, brain CT or MRI, Doppler ultrasound of brachiocephalic arteries; if necessary, 24-hour ECG monitoring and esophagogastroduodenoscopy).
During hospitalization, all patients underwent training at the “Rehabilitation school”, the program of which included classes devoted to raising the awareness of patients and their relatives about AF and CES, the formation of recovery motivation, the implementation of physician’s recommendations, the acquisition of skills for self-monitoring, proper nutrition, adequate exercise, cessation of bad habits. At the time of discharge, all patients were selected for the optimal individualized drug therapy.
Before discharge from the hospital, all patients signed an informed consent, after which they were randomized into two groups using a random number method. Patients of the group I (experimental) (n=72) were followed up for one year in accordance with a specially developed comprehensive ambulatory monitoring system. This system included not only a rehabilitation program created individually for each patient in accordance with his clinical characteristics, but also regular monthly visits to physician, during which a complex of diagnostic investigations was carried out. At each visit, complaints, symptoms and medical adherence were assessed, and, if necessary, were adjusted. Also, the doctor talked with the patient and his relatives about the need to comply with the recommended regimen and taking medications, supporting the motivation for treatment. Patients of group II (control) (n=67) were followed up at the primary care level in accordance with the current program, and a control visit to was performed for them once — after 12 months.
The primary efficacy endpoint was the combination of myocardial infarction (MI), ischemic stroke, and cardiovascular death; the secondary efficacy endpoints were all-cause mortality and hospitalization for decompensated HF. The primary safety endpoint was an episode of major or clinically relevant non-major bleeding according to the International Society on Thrombosis and Haemostasis (ISTH) classification.
Statistical analysis was carried out using IBM SPSS Statistic 22.0 (IBM, USA), Statisticа 10.0.228.8, Excel-2013, Access-2010, Word-2010 (Microsoft Corp., USA). Differences were considered significant at p<0,05; at p?0,01 — very significant; at p?0,001 — highly significant.
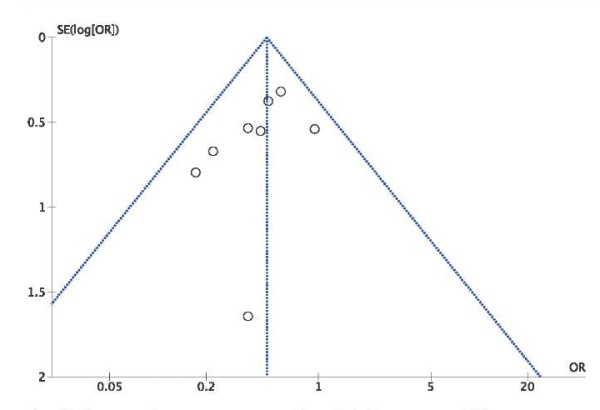
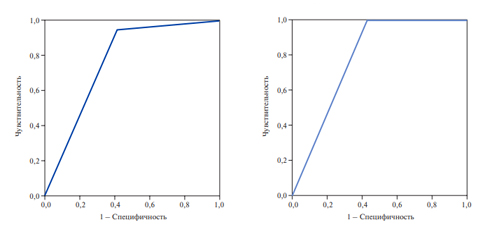
The study used the receiver operator characteristic analysis (ROC-analysis), which allows to classify positive and negative examples. Its graphical interpretation was the ROC curve, which reflects the results of binary classification and shows the dependence of correctly classified positive examples on the number of incorrectly classified negative examples. A quantitative interpretation was provided by the area under ROC curve (AUC). It is generally accepted that the AUC coefficient, which is in the range of 0,9-1,0, reflects the excellent quality of model; 0,8-0,9 — very good; 0,7-0,8 — good; 0,6-0,7 — sufficient; 0,5-0,6 — poor quality. The chi-square test was used to test the independence of categorical variables in crosstable. The strength of the relationship between exposure and disease was assessed by odds ratio (OR) of event incidence in the comparison groups. With OR >1, the probability of an outcome in the experimental group is higher than in the control group. Moreover, the higher the OR value, the higher the probability of event development. With OR <1, the probability of an outcome in the study group is lower than in the control group.
Results
At the first statistical analysis stage, the groups of randomized patients were assessed for normal distribution. Due to the fact that traits in these groups were non-normally distributed, for their comparison we used the Kolmogorov-Smirnov test. Data on the age patterns, main anthropometric parameters, sex, comorbidity prevalence, main risk factors for CVD, AF type, presence of prior bleeding events, with intergroup comparison, are presented in Tables 1 and 2.
Table 1
Patterns of the compared groups by age and main anthropometric parameters*
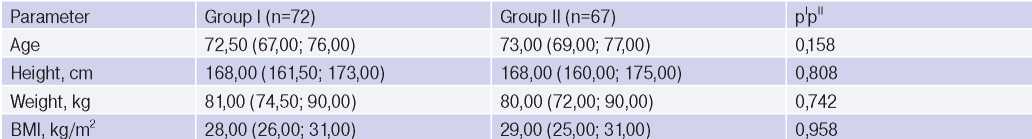
Note: * — parameters are presented as median (Me) and interquartile range (Q1-Q2).
Abbreviation: BMI — body mass index.
Table 2
Patterns of the compared groups by sex, comorbidity profile, CVD risk factors, AF type, history of bleeding
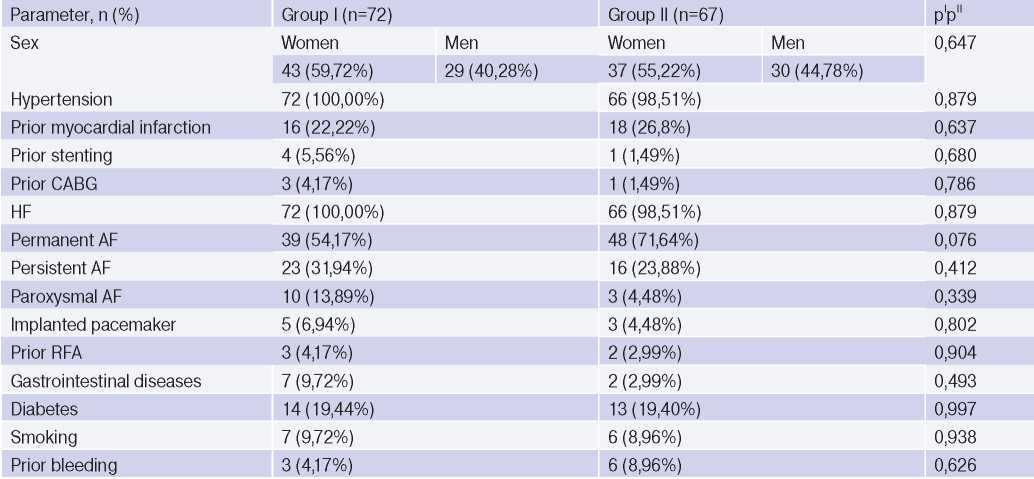
Abbreviations: MI — myocardial infarction, CABG — coronary artery bypass grafting, RFA — radiofrequency ablation, CVD — cardiovascular diseases, AF — atrial fibrillation, HF — heart failure.
Thus, the experimental and control groups at the time of randomization were comparable in age, main anthropometric parameters, sex, comorbidity prevalence, AF type, and a history of bleeding events.
At baseline, the groups were compared in terms of the risk of thromboembolic and bleeding events using the CHA2DS2-VASc and HAS-BLED scores, respectively, which did not reveal significant differences (Table 3).
Table 3
Patterns of the compared groups by risk of thromboembolic and bleeding events*
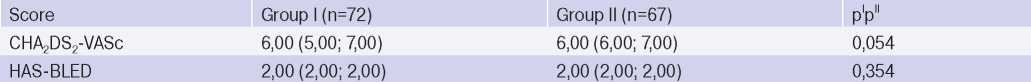
Note: * — parameters are presented as median (Me) and interquartile range (Q1-Q2).
At the time of discharge, the groups were comparable in all main statistical characteristics, which rule out the possible influence of the latter on the study outcomes.
Based on 1-year follow-up, an incidence of endpoints was compared between groups I and II (Table 4).
Table 4
Incidence of endpoints (cardiovascular death, MI, stroke) in the compared groups
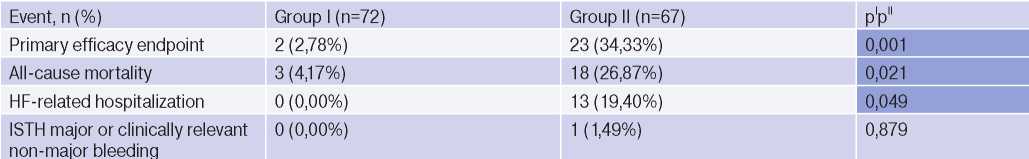
Abbreviations: HF — heart failure, ISTH — International Society on Thrombosis and Haemostasis.
After 12 months of outpatient rehabilitation, the compared groups significantly differed in the incidence of the following events: the primary composite efficacy endpoint (cardiovascular death, MI, and ischemic stroke) and two secondary efficacy endpoints (all-cause mortality and HF-related hospitalization), which in group I patients were observed less frequently. At the same time, there were no differences in the incidence of the primary safety endpoint between the groups.
In addition, in group II, a relationship was found between the death and no anticoagulant therapy (OR 7,68; 95% confidence interval, 1,59-37,03; p=0,01). The ROC analysis confirmed the relationship between no anticoagulant therapy and death, while the regression quality corresponded to good (AUC 0,77; sensitivity 94,74%; specificity 59,17%) (Figure 1).
We also found a relationship in group II between decompensated HF and no diuretic intake (?2 — 7,38, p=0,007). According to logistic regression analysis of decompensated HF, the prognostic significance of diuretic therapy was shown, while the regression quality corresponded to good (AUC 0,783; sensitivity 100%; specificity 57,14%) (Figure 2).
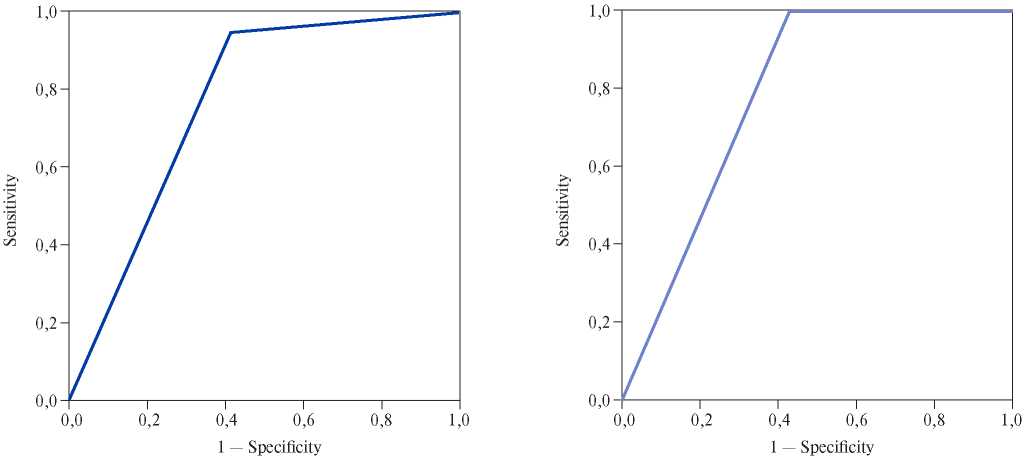
Figure 1. Analysis of the relationship between no anticoagulant therapy and death.
Figure 2. Analysis of the relationship between no diuretic therapy and HF decompensation within 12 months.
In group I, during 12-month outpatient followup, a significant proportion of patients required changes in the drug therapy prescribed at hospital discharge. This could be a drug replacement, a decrease or increase in dose, the addition of another drug with a different mechanism of action to enhance the effect. For example, alteration of antihypertensive therapy was required in 34 patients (47,22%), anticoagulant therapy — in 13 patients (18,06%). Most often, a dose change was required in warfarin therapy — out of 12 people taking it, 8 had an instability in international normalized ratio level. However, in the end of 1-year follow-up, adherence to anticoagulant and antihypertensive therapy in group I was 100%. Correction of HF therapy was required in 24 patients (33,33%), while not a single patient of group I during our study was hospitalized due to decompensated HF.
In group II, antihypertensive drugs were taken by 53 (79,10%), anticoagulants — 26 (38,81%), and adequate HF therapy — 13 (19,40%) patients, which, of course, influenced the incidence of endpoints.
Discussion
The importance of secondary stroke prevention is currently not in doubt. Over the years, the approach to long-term management of stroke patients has undergone dramatic changes. Currently, stroke patients, including those after CES, receive a list of recommendations for further treatment upon discharge, which consists of non-drug and drug measures for the secondary prevention of recurrent stroke and other cardiovascular events.
Drug therapy in such patients, as a rule, consists of several classes of drugs. Life-long anticoagulant prophylaxis of TEE is of paramount importance in patients with AF after CES [1][6]. In addition, it is necessary to assess the rationale of antiarrhythmic drug therapy, depending on the chosen strategy for controlling the rhythm or heart rate. The need to take other medicines is specified by comorbidity profile. For example, the vast majority of patients with AF require antihypertensive therapy. Thus, in the population of patients included in our study, the prevalence of hypertension reached 100% in group I and 98,51% in group II. The choice of an antihypertensive drug largely depends on the comorbidity status of a particular patient, and often a combination of antihypertensive drugs is required. The presence of coronary artery disease in a patient, depending on its course, may require intensifying antithrombotic therapy, which increases the risk of bleeding events. In addition, within the secondary prevention, treatment of HF and diabetes should be carried out. Hepatic and renal dysfunction must also be taken into account when choosing specific drugs, due to a possible change in their pharmacokinetic parameters.
All these factors are assessed and taken into account when planning an inpatient treatment and formulating recommendations at discharge. Further, at the outpatient stage of management, a periodic reassessment of clinical symptoms and some investigational parameters is required. For example, taking warfarin requires mandatory monthly determination of the international normalized ratio, and taking antiarrhythmic drugs requires regular assessment of the QT interval on the ECG. All patients with AF require renal function monitoring, the regularity of which depends on the initial value of the glomerular filtration rate of a particular patient and is calculated using a special equation. In addition, it is necessary to regularly reevaluate the risks of thrombotic and bleeding events, as well as the balance of benefits and risks from the treatment. All these features of the management of AF patients are reflected in modern guidelines [1][6], and the prognosis of patients’ life directly depends on its optimal implementation.
The implementation of this program of secondary prevention of CES in full is possible only with regular follow-up by a specially trained specialist. The rationale of widespread implementation of this approach to the outpatient rehabilitation is also evidenced by our study — patients followed up in accordance with comprehensive ambulatory monitoring system within a year after discharge had a significant decrease in the primary composite endpoint (cardiovascular death, MI, ischemic stroke), as well as such secondary efficacy points as all-cause mortality and HF-related hospitalization.
Regular monthly visits to a specialist made it possible to timely adjust the treatment, as well as maintain a high level of medical adherence, which in group I reached 100%. A number of studies have been published confirming that it is the high medical adherence that can influence the prognosis of patient life [8][9][10][11]. However, to date, the quality of outpatient management of stroke patients remains insufficient [10][12][13]. According to our own data published earlier, adequate prevention of TEE in actual clinical practice is extremely rare — only in 16,2% of AF patients, outpatient physicians recommended taking anticoagulants [14]. Non-compliance with modern guidelines for outpatient management can be explained by significant workload of doctors, as well as, possibly, insufficient awareness of modern approaches to treatment.
Conclusion
Based on the above, we believe that comprehensive ambulatory monitoring program for AF patients after CES has proven high effectiveness, and its widespread practice is an urgent task of modern healthcare. The approaches to the outpatient management of AF patients after CES should be globally reviewed. It seems relevant to create ambulatory offices for the secondary prevention of stroke, which will deal with the adjustment of risk factors, the selection of optimal drug therapy and monitoring of medical adherence.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Efimova O.I., Pavlova T.V., Pyscheva L.V., Khokhlunov S.M. Effectiveness of a comprehensive ambulatory monitoring system for patients with atrial fibrillation after cardioembolic stroke. Russian Journal of Cardiology. 2021;26(1S):4402. (In Russ.) https://doi.org/10.15829/1560-4071-2021-4402
Copy