Оценка отдаленных симптомов у пациентов с постпульмональным эмболическим синдромом с помощью показателей исходов, сообщаемых пациентами
Аннотация
Пациенты после перенесенной тромбоэмболии легочной артерии (ТЭЛА) имеют повышенный риск развития хронических осложнений, несмотря на использование антикоагулянтной терапии. Сочетание одышки, сниженных функциональных возможностей, правожелудочковой недостаточности, хронической тромбоэмболической легочной гипертензии или хронической тромбоэмболической болезни легких является частью термина «постпульмональный эмболический синдром»(post-pulmonary embolic syndrome). Симптомы этой патологии могут существенно влиять на качество жизни. Для улучшения общего состояния пациентов с острой ТЭЛА необходима ее адекватная диагностика и разработка стратегии борьбы с отдаленными последствиями.
Целью данного исследования является попытка дать определение постпульмональному эмболическому синдрому и рассмотреть возможность использования показателей исходов, сообщаемых пациентами (ПИСП) для оценки их функциональных возможностей.
Поиск статей в PubMed, опубликованных за последние 5 лет, осуществлялся с использованием следующих ключевых слов: post-pulmonary embolism syndrome; symptoms; PROMs; score; quality of life; dyspnea. Повторные публикации были исключены. Данные из найденных статей обобщены в текущем обзоре.
Перевод в разработке
Introduction
Despite the fact that pulmonary embolism (PE) is a potentially fatal pathology, early mortality related to PE is progressively decreasing [1]. However, the picture is not entirely positive for survivors of PE. Studies indicate that about half of those are unable to fully regain their previous level of functioning. Many survivors report experiencing long-lasting and sometimes severe symptoms or disabilities. These patients continue to experience symptoms such as dyspnea, impaired functional status, and reduced exercise capacity. These limitations significantly impact their quality of life for many years after the event [2]. As a result, ensuring a good functional status and quality of life (QoL) for these individuals will require continued research and healthcare efforts to improve the outcomes and well-being of PE survivors.
The management of symptomatic patients survivors after PE can pose significant challenges for physicians and the healthcare system. This situation also carries the risk of incurring substantial costs. Certain patients require long-term medication or costly investigations, while others may face difficulties returning to the workforce [3]. In recent years, a series of publications have emerged that focus on the systematization of patients after pulmonary embolism, offering diagnostic and treatment algorithms, along with different scores to assess and objectively measure their functional impairments, such as patient-reported outcome measures (PROMs) [4][5].
The Task Force (European Society of Cardiology — ESC; European Respiratory Society — ESR) recommendation about optimal follow-up after acute pulmonary embolism, 2022 doesn’t recommend routine follow-up of asymptomatic PE patients by imaging methods but suggests evaluating the index imaging test used to diagnose acute PE for signs of chronic thromboembolic pulmonary hypertension (CTEPH), hence the importance of assessing the symptoms of patients after acute PE [6].
Properly managing survivors of PE requires a crucial awareness of Post-Pulmonary Embolic Syndrome (PPES). The concept of PPES was described in 2014 by Klok, et al. [7]. It is further characterized as the presence of new or progressive dyspnoea, a decrease in exercise tolerance, and/or an unexplained impairment of functional or mental status persisting for at least three months after an acute episode of pulmonary embolism, despite receiving adequate anticoagulant treatment and inexplicable by other comorbidities.
PPES is defined as the presence of any of the following, summarised in table 1 [6]:
- chronic thromboembolic pulmonary hypertension (CTEPH);
- chronic thromboembolic pulmonary disease (CTEPD) without pulmonary hypertension (PH);
- post-PE cardiac dysfunction — characterized as persistent right ventricle impairment after PE;
- post-PE functional impairment.
Table 1
The main characteristics of PPES, acording [6]
| Parameter | Mechanism | Characteristics | Diagnostics | Impact |
| CTEPH | unresolved thrombi | • mismatched perfusion defects on ventilation/perfusion (V/Q) test,
• elevated pulmonary pressure, measured with a right heart catheterization, according to the European Society of Cardiology (ESC) guideline criteria [8] |
• screening algorithm «CTEPH rule-out criteria»[9],
• Certain index computed tomography pulmonary angiography performed to confirm the PE was proposed to predict a future CTEPH diagnosis [10], • Echocardiography, • V/Q scanning, • cardiopulmonary exercise test, • Right heart catheterization |
an early diagnosis will lead to improved survival and better QoL |
| CTEPD without PH | unresolved thrombi | All items:
1. exertional dyspnea of the New York Heart Association (NYHA) class II, 2. persistent thromboembolic material in the pulmonary artery tree despite 3 months of adequate anticoagulant therapy, 3. normal mean PAP at rest, 4. dead space ventilation as determined by cardiopulmonary exercise test and/or PH during exercise |
• Echocardiography,
• V/Q scanning, • cardiopulmonary exercise test, • Optionally Right heart catheterization (excluding CTEPH) |
identifying potential CTEPD without PH is important because targeted treatment in CTEPH expertise centers could improve QoL and functional outcomes. Currently, it is unknown whether CTEPD without PH may progress to CTEPH, and if so, how often this occurs |
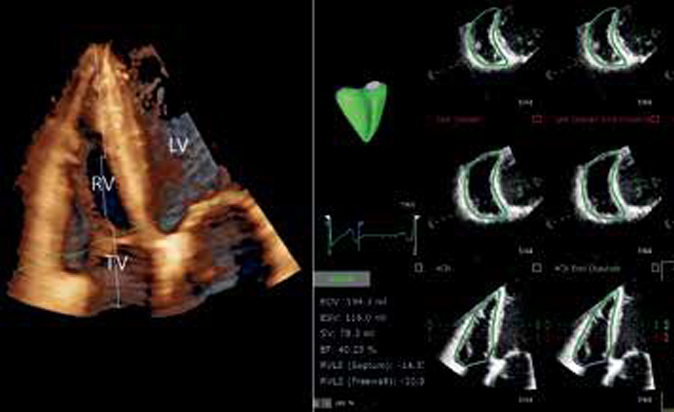
| Post-PE cardiac dysfunction | possible, myocardial fibrosis | • presence of intermediate/high echocardiographic probability of PH according to the European Society of Cardiology (ESC) criteria [8],
• RV hypokinesis, or RV dilatation, • exertional dyspnea (NYHA II-IV) |
• NT-proBNP,
• Echocardiography, • cardiopulmonary exercise test, • Cardiac Magnetic Rezonance |
improve outcome and right heart failure |
| Post-PE functional impairment | decreased daily physical activity — deconditioning | • persistent dyspnea,
• exercise intolerance, and/or • diminished functional status after an acute PE with no apparent non-PE — related alternative explanation for the functional status after an acute PE with no apparent non-PE — related alternative explanation |
• cardiopulmonary exercise test,
• PROMs |
post-PE functional impairment is associated with reduced QoL and higher prevalence of depression and permanent work-related disability |
The most concerning subgroup of PPES is CTEPH, and it takes precedence to evaluate the possibility of its presence. There is a dedicated algorithm designed for the efficient detection of these concerning complications [11].
However, the majority of PPES patients are ultimately diagnosed with post-PE functional impairment. Utilizing PROMs can be helpful in objectively assessing complaints after acute PE and identifying patients who may require further evaluation for outcome optimization.
Post-PE functional impairment and Long-term Symptoms in PPES
The most common typical symptoms in PPES patiens are: pain, anxiety, depression, fatigue, dyspnoea.
Table 2
The most recommended PROMs in PPES functional impairment evaluation
| PROMs | Parameter | Item | Studies |
| PVFS — Post-VTE Functional Status [12] | Symptoms, pain, anxiety | 6 | [13][14] |
| Medical Research Council dyspnea Scale, original or modified (mMRC)1 | Dyspnea | 5/4 | [15] |
| The modified Borg Dyspnea Scale2 | Dyspnea | 10 | [16] |
| the World Health Organization Functional Class [8] | Dyspnea, fatigue, pain | 4 | [17] |
| PEmb-QoL (the validated Pulmonary Embolism Quality in Life)3 | QoL | 9 | [18] |
| PROMIS Short Forms for pain and Dyspnea Severity4 [22] | Pain and dyspnea | various | [19] |
| The Checklist Individual Strength with fatigue severity (CIS-Fatigue) [20] | Fatigue | 8 | [21][22] |
| Patient Health Questionnaire-9 (PHQ-9)5 | Depression | 9 | [23][24] |
| Generalized Anxiety Disorder-7 (GAD-7)6 | Anxiety | 7 | [25] |
| Hospital Anxiety and Depression Scale7 | Depression and anxiety | 14
(7 depresion/7 anxiety) |
[26] |
PROMs in PPES functional impairment evaluation, according [4].
The post-VTE functional status is intended to be assessed [4]:
- at the time of discharge after a VTE diagnosis,
- after 3 months, and
- optionally after 12 and/or 24 months following a VTE diagnosis to check for recovery and degree of persisting disability.
Dyspnea
Dyspnea is one of the most common symptom of patients with PE and majority of respiratory conditions. Dyspnea is a frequent complaint after a PE, despite adequate anticoagulation, and these may persist for a long period after acute PE independent of concomitant dyspnea-related comorbidities [27].
Though dyspnea (widely known as breathlessness) is subjective and difficult to quantify its plays a major role in decision-making about diagnosis and treatment so it is important to measure the amount of dyspnea. For standardized evaluation of the severity of dyspnea, the modified Medical Research Council (mMRC) dyspnea scale may be applied in PE patients [19]. Alternative PROMs are PROMIS Short Form Dyspnea Severity, the (modified) Borg Dyspnea Scale, and the World Health Organization functional class.
MRC and MRCm (Medical Research Council dyspnea Scale, modified). MRC was published in 1959, the latest version being published in 1986. The scale on original MRC dyspnoea scale is very simple, consisting of just five items containing statements about the impact of breathlessness on the individual and leading to a grade from 1 to 5. It can be self-administered or with a slight change in the format of questions, delivered by a researcher or clinician. Either way, it takes seconds to complete.
In the self-administered format, the patient selects the option that best describes their breathlessness as it affects their function. It does not grade breathlessness itself but the functional impact of breathlessness and perceived limitations that result. The mMRC breathlessness scale ranges from grade 0 to 4. It is very similar to the original version and is now widely used in studies [28].
Modified Borg Dyspnoea Scale (MBS). The original scale was developed in healthy individuals to corre late with exercise heart rates and to enable subjects to better understand the terminology in 1982. The category ratio scale was later developed and has since also been modified to more specifically record symptomatic breathlessness (Modified Borg Dyspnoea Scale). MBS is a 0 to 10 rated numerical score used to measure dyspnea as reported by the patient during submaximal exercise and is routinely administered during six-minute walk testing (6MWT), one of the most common and frequently used measures to assess disease severity in PAH. The MBS is reproducible within a single testing period and tracks with objective indices of exercise intensity in healthy controls and thus has been extrapolated for use in chronic lung disease [29].
The World Health Organization functional classification (WHO-FC) is a tool used to measure disease severity in patients with PAH whereby healthcare providers use patient reports of symptom experience and activity limitations to make their assessment. The WHO-FC was adapted in 1998 for use with patients with PAH based on the New York Heart Association (NYHA) classification, a 4-point index of functional status of patients with HF. Patients assessed by the WHO-FC are allocated into class I, II, III, or IV; a higher class is indicative of more severe disease (i. e., greater functional impairment) [30].
Pain
Such disorders as pain associated with anxiety could lead to less physical activity, with deconditioning and psychogenic functional limitation [31].
To assess pain severity, PROMIS Short Forms for pain can be applied. The PROMIS (Patient-Reported Outcomes Measurement Information System) was established in 2004 with funding from the National Institutes of Health (NIH). The initiative focused on the development and psychometric evaluation of multiple-item banks for assessing health domains, including pain-related outcomes. The PROMIS network investigators developed item banks and measures for pain interference, pain behavior, pain quality, and pain intensity. Although broad item banks were developed to assess pain interference and behavior, sets of relevant items were developed for assessing pain intensity and pain quality — the PROMIS shorts forms. The pain-related measures and other PROMIS measures (eg, fatigue, physical function, social function, depression, etc.) also might be applicable to pain studies. The PROMIS pain-related pain measures have the potential to improve the measurement of pain interference and behavior, and other outcomes, and to increase our understanding of the effects of pain on patients’ lives and function, and of the effects of treatment interventions [32].
PROMIS is used in the quantification of chronic diseases, including respiratory diseases [33].
Anxiety and depression
Mental health problems such as depression, anxiety and panic syndrome that are related to venous thromboembolism are not negligible, contributing to functional deterioration after pulmonary embolism [3].
Anxiety and depression are a frequent finding in PPES patients. About one in five of them may have these symptoms, even more than 2 years after the acute episode. Patients with depressiveness 3 months after PE were found to be significantly older, had a higher simplified pulmonary embolism severity index (sPESI), higher education level, more frequently previous depression, lower oxygen saturation, and a longer hospital stay [26]. Identifying patients who require psychological counselling and treatment for depression or panic disorders, appears to have an incremental benefit for patients with pulmonary embolism [34].
Psychological well-being can be assessed using the Patient Health Questionnaire-9 for depression and Generalized Anxiety Disorder-7 for anxiety, or the Hospital Anxiety and Depression Scale.
Patient Health Questionnaire- 9 (PHQ-9) was originally published in 1999 in the Journal of the American Medical Association. The PHQ-9 is used to screen for depression and assess its severity.
The PHQ-9 consists of 9 questions. The patient self-reports depression-associated symptoms according to their frequency in the past 2 weeks. The score is calculated by summing the response values for each of the 9 questions.
The minimum score of 0 indicates no self-reported symptoms of depression. The maximum score of 27 indicates the most severe depression. The following correspondence between PHQ-9 score and depression severity has been proposed: 0-4: None-minimal, 5-9: Mild, 10-14: Moderate, 15-19: Moderately Severe, 20-27: Severe [35].
The Generalized Anxiety Disorder 7-item scale (GAD-7) was originally published in 2006 in the journal Archives of Internal Medicine. It is designed to be used as a brief screening questionnaire for generalized anxiety disorder.
The measure consists of 7 questions that relate to symptoms of anxiety disorder. Each question is scored from 0-3, with higher scores indicating greater anxiety- associated symptoms. The maximum score is 21 and the minimum score is 0.
Scores greater than 10 may warrant further investigation for the possibility of anxiety disorder (moderate to severe anxiety). Scores greater than 15 indicate severe anxiety [36].
Hospital Anxiety and Depression Scale (HADS) is a screening tool that quickly and effectively identifies patients that show symptoms of depression and/or anxiety, has developed in 1983. Its use in the healthcare setting increased over time, since it evaluates cognitive, emotional, and behavioral symptoms, excluding physical symptoms. Thus, it avoids possible false positives and excludes symptoms associated with severe mental disorders. Once patients are identified as having possible symptoms of depression and/or anxiety, they can be selected for diagnostic confirmation. The HADS has fourteen-item scale that generates of which seven items relate to anxiety and the other 7 relate to depression. Interpretation: 0-7 = Normal, 8-10 = Borderline abnormal (borderline case), 11-21 = Abnormal (case) [37].
Fatigue
The Checklist Individual Strength (CIS) was developed by the Dutch research team in 1994. The questionnaire consisted of 24 items and analysis indicated 4 components: Subjective fatigue (8 items), Concentration (5 items), Motivation (4 items), and Physical activity (3 items).
The CIS-Fatigue reports on fatigue severity and consists of eight items scored on a seven-point Likert scale. The score ranges from 8 to 56, with higher scores indicating more severe fatigue. Severe fatigue is indicated by a CIS-Fatigue score ≥35 points, a validated cutoff score. Chronic fatigue was defined as severe fatigue (CIS-Fatigue score ≥35 points) lasting at least 6 months according to self-report [22].
Disease specific PROMs
The PVSF scale is the most used questionnaire for scaling dyspnea in patients with post-PE syndrome. This scale is ordinal, has 6 steps ranging from 0 (no symptoms) to 5 (death, D), and covers the entire range of functional outcomes by focusing on limitations in usual duties/ activities either at home or at work/study, as well as changes in lifestyle. The scale grades are intuitive and can easily be grasped by both clinicians and patients.
The post-VTE functional status is intended to be assessed: (1) at the time of discharge after a VTE diagnosis, (2) after 3 months, and (3) optionally after 12 and/or 24 months following a VTE diagnosis to check for recovery and degree of persisting disability. The 3-month follow-up corresponds to a routine visit performed by the treating physician for determination of the duration of anticoagulant treatment. The last time point is chosen as the functional status is expected to be stabilized in most patients and because it is the optimal moment for considering the presence of severe VTE complications, such as chronic thromboembolic pulmonary hypertension (CTEPH). The persistence of symptoms or an incomplete functional recovery after acute pulmonary embolism should trigger diagnostic tests to rule out CTEPH.
The Pulmonary Embolism Quality of Life (PEmb-QoL) questionnaire was developed and validated as a disease specific instrument to measure QoL in survivors of acute PE It was proposed in 2009 and was originally written in Danish, later translated into English and other languages. It contains nine subsections with various questions for the patient to answer [38].
According to the World Health Organisation (WHO), quality-of-life is defined as individuals’ perceptions of their position in life in the context of the culture and value systems in which they live, and in relation to their goals, expectations, standards and concerns. This concept has gained considerable importance over the last 30 years, enabling an improvement in patients’ medical, social and economic care.
Deconditioning
One of the primary reasons for the reduced functional capacity in patient post PE is attributed to the decline in daily physical activity, leading to physical deconditioning.
Deconditioning is defined as a loss of physical fitness due to failure to maintain an optimal level of activity or training8. Inactivity of any origin can lead to deconditioning, and in the patient with pulmonary embolism, the decrease in functional capacity is obtained by the vicious circle, represented by pain, anxiety, depression, dyspnea, together generating the lack of physical activity [39]. In the prospective ELOPE study, it was suggested for the first time that the deconditioning that occurs after acute pulmonary embolism appears to be the most likely explanation for the limitation of physical activity, mostly impaired circulatory or ventilatory function. Exercise limitation on 1-month cardiopulmonary exercise test was predictive of worse functional outcome during follow-up, suggesting that identifying exercise-limited patients early after pulmonary embolism is of prognostic value, and that exercise rehabilitation interventions early after pulmonary embolism may have potential to improve long-term functional outcomes. In adition it was desribed other risc factors for [2]. The role of inactivity was also highlighted in a cohort of intermediate- and high-risk pulmonary embolism patients, in which no significant association was found between patient-reported symptoms, pulmonary function, right ventricular dysfunction, and changes from cardiopulmonary testing [40]. Thus, the authors suggest that functional impairment appears to be attributable to general deconditioning rather than intrinsic cardiopulmonary limitation, and rehabilitation plays an important role for improving patient outcomes and quality of life. This even though physical activity and physical exercise are known factors that increase fibrinolysis and are used as part of the management of many cardiopulmonary diseases [41]. Other studies have also demonstrated clinical improvement after exercise training, further emphasizing the contribution of deconditioning in PPES. Pulmonary rehabilitation is a comprehensive intervention program that combines multiple measures and disciplines, including but not limited to exercise training, education and behavioral changes, such as: Exercise training, Respiratory training, Respiratory training, Health education, Psychological intervention, Nutritional supplementation [42]. The existing evidence suggests that pulmonary rehabilitation is a potential treatment for alleviating post-PE syndrome, which improves the quality of life and prognosis of patients with PE [43].
Conclusion
After an episode of pulmonary embolism, a large number of patients remain with functional limitations and persistent symptoms. Multiple studies and metaanalysis demonstrated that it is essential to diagnose PPES earlier in order to have better long-term outcomes. The evaluation of symptoms is very important for the assessment of the population that needs to be followed in the long term, and the specific validated scores are essential tools for detecting and monitoring patients who require specific medical intervention.
There are algorithms proposed to objectify the symptoms after an episode of pulmonary embolism and to contribute to the correct and timely selection of patients with PPES who require additional evaluations and specialized treatment. Additionally of medicinal treatment, exercise training programs — rehabilitation and psychological support for the remediation of anxiety and depression could contribute to patients’ functional recovery and significant improvement of their quality of life.
Future directions: It would be beneficial to conduct randomized studies comparing PROMs to determine the most practical assessment and monitoring tools for patients with PPES, with the aim of enhancing their quality of life.
Relationships and Activities. This research was part of the project No 20.80009.8007.28 «Strategic approach to pulmonary embolism in the pre- and post-hospitalization period in the Republic of Moldova», within the State Program of the Republic of Moldova (2020-2023).
1. MRC Dyspnoea Scale — UKRI [Internet]. [cited 2023 Jul 24]. Available from: https://www.ukri.org/councils/mrc/facilities-and-resources/find-an-mrc-facility-or-resource/mrc-dyspnoea-scale/.
2. Resources | Heart Online [Internet]. [cited 2023 Jul 24]. Available from: https://www.heartonline.org.au/resources.
3. Official PEmb-QoL distributed by Mapi Research Trust | ePROVIDE [Internet]. [cited 2023 Jul 24]. Available from: https://eprovide.mapi-trust.org/instruments/pulmonary-embolism-quality-of-life-questionnaire#need_this_questionnaire.
4. PROMIS [Internet]. [cited 2023 Jul 24]. Available from: https://www.healthmeasures.net/explore-measurement-systems/promis.
5. The Patient Health Questionnaire (PHQ-9) — NeurologyToolKit [Internet]. [cited 2023 Jul 24]. Available from: https://neurotoolkit.com/phq-9/.
6. Free Online GAD-7 Score Calculator — NeurologyToolKit [Internet]. [cited 2023 Jul 24]. Available from: https://neurotoolkit.com/gad-7/.
7. Awell Score [Internet]. [cited 2023 Jul 24]. Available from: https://score.awellhealth.com/calculations/hads/.
8. Deconditioning | definition of deconditioning by Medical dictionary [Internet]. [cited 2023 Jul 24]. Available from: https://medical-dictionary.thefreedictionary.com/deconditioning.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Ключевые слова
Для цитирования
Diaconu N., Sorici G., Civirjic I., Grosu A. Оценка отдаленных симптомов у пациентов с постпульмональным эмболическим синдромом с помощью показателей исходов, сообщаемых пациентами. Российский кардиологический журнал. 2023;28(4S):5543. https://doi.org/10.15829/1560-4071-2023-5543. EDN: AJZOCU For citation:
Скопировать