Takotsubo syndrome in a patient with atrial fibrillation after electrical cardioversion: a case report

Takotsubo syndrome is a condition characterized by reversible stress-induced left ventricular (LV) systolic dysfunction. Despite the dominant prevalence of the apical variant (81,7%), in recent years there has been more and more data on the development of the midventricular (14,6%), basal (2,2%), and extremely rarely focal type (1,5%) [1]. Despite the fact that takotsubo syndrome occurs predominantly in postmenopausal women, ~9% of cases have been described in males [2]. The true prevalence of takotsubo syndrome is unknown, which is associated with the specifics of differential diagnosis, which is often inaccessible to a non-specialized institution. However, in 1-2% of all cases of hospitalization with a primary diagnosis of acute coronary syndrome (ACS), takotsubo syndrome is detected [3]. Despite the reversibility of functional myocardial disorders, the incidence of cardiogenic shock and death in takotsubo syndrome in the International takotsubo registry, which included 1750 patients, was comparable to that in ACS [4].
This paper presents a clinical case of takotsubo syndrome in a patient with atrial fibrillation (AF) who underwent electrical cardioversion.
Case report
A 68-year-old man was transported to a cardiology center with paroxysmal AF with complaints of arrhythmic heartbeat with a heart rate of up to 160 bpm, weakness, pressing chest pain, and shortness of breath for the last 28 hours.
There was prior acute myocardial infarction. According to coronary angiography (CAG) 3 years ago, coronary artery stenosis was not detected. AF episodes was registered last 3-5 years and are almost always clinically accompanied by the development of chest pain. The patient regularly took rivaroxaban 20 mg, atorvastatin 20 mg, egilok 12,5 mg (low dose due to tendency to hypotension), and omeprazole. Appointment of antiarrhythmic therapy at the prehospital stage was limited by the development of sinus bradycardia. According to echocardiography, performed 6 months ago during sinus rhythm, LV ejection fraction (EF) in B-mode was 69% without local contractility disorders, left atrium — 48 mm, end diastolic volume — 124 ml, end systolic volume — 38 ml, LV mass — 239 g, mitral valve prolapsed — 5 mm with grade 2 regurgitation.
Paraclinical data
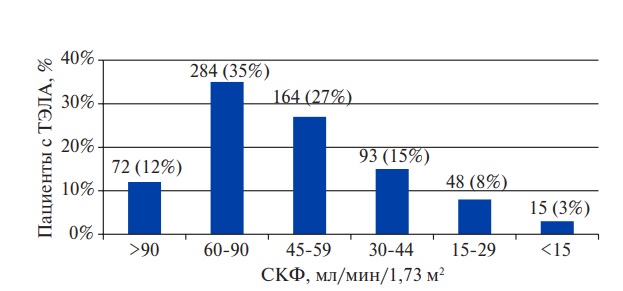
Electrocardiography (ECG) at admission revealed AF with a heart rate of 155 bpm, horizontal ST segment depression up to 0,5 mm in V3-V6 (Figure 1 A).
Taking into account the chest pain, ACS was initially excluded. Due to the ineffectiveness of the chemical cardioversion, he was hospitalized to restore sinus rhythm.
Data of objective status and laboratory testing at admission were without clinically significant abnormalities.
During hospitalization, additional information was obtained about an echocardiography performed 2 days before admission to the hospital against the background of tachysystole of 125 bpm (which indicated an unspecified duration of AF during hospitalization, despite acute complaints, and served as the basis for stopping chemical cardioversion), where EF was 55% with slight diffuse hypokinesia and hydropericardium <100 ml.
Due to the ineffectiveness of chemical cardioversion with cordarone, which continued during the first day of hospitalization, tachysystole up to 150 bpm, weakness, chest pain, on the third day of admission after preliminary transesophageal echocardiography and exclusion of atrial blood clots, electrical cardioversion with a 200 J biphasic shock wasperformed. Sinus rhythm was restored. HR was 54 bpm, ST segment — on the isoline, T wave inversion in III lead, QT of 520 ms, QTc of 493 ms (Figure 1 B). A clinical improvement was achieved, and a beta-blocker was retained in the treatment to correct the prolonged QT interval.
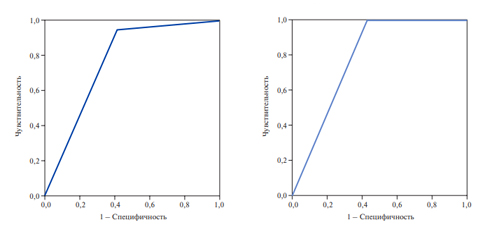
Transthoracic echocardiography after sinus rhythm restoration on the third day of hospitalization revealed a significant decrease in LV contractility, EF in B-mode of 32%, diffuse hypokinesia, grade 2 mitral valve regurgitation, dilatation of the left atrium to 52 mm (140,6 ml) in anterior-posterior size and the LV (end systolic dimension, 49 mm, end diastolic dimension, 55 mm), moderate pulmonary hypertension (right ventricular systolic pressure, 47 mm Hg), bilateral hydrothorax up to 150 ml on the left and 170 ml on the right, hydropericardium (55- 60 ml) (Figure 2). Given the significant unfavorable changes over the past 5 months, myocardial scintigraphy with 99mTc-technetrile with a stress test was performed on the 4th day, revealing a slight defect in the radiopharmaceutical accumulation (<5%) in the middle sections of LV anterior and posterior walls. At the same time, during the cycle ergometry, the patient noted the development of a pronounced retrostenal pain in the absence of ECG changes, which caused the load termination.
Elective ECG on the 5th day revealed sinus rhythm, heart rate of 56 bpm, the appearance of a negative T wave in V1-V3 with the preservation of changes over the next 4 days. QT was 600 ms, QTc — 589 ms (Figure 1 C).
CAG detected stenosis up to 25% in the proximal and middle segments of the right coronary artery and obtuse marginal artery; coronary blood flow was slowed down. In view of the negative ECG dynamics, differential diagnosis with ACS was again carried out, but no convincing data were obtained. The dynamics of the levels of specific cardiac markers during the period of hospitalization is shown in Table 1.
On day 6, transthoracic echocardiography was performed. Positive dynamics was noted in the form of a significant improvement in global contractility up to 48%, but the preservation of local disorders in the form of akinesia of the anterior septal segments of the basal-middle localization, hypokinesia of the apical segments of the same localization. Bilateral hydrothorax regressed to 110 ml, hydropericardium was minimal (Figure 3).
ECG on day 12 showed sinus rhythm, heart rate of 54 bpm, ST segment on the isoline, T wave inversion in III, QT of 480 ms, and QTc of 463 ms (Figure 1 D).
Heart failure compensation was achieved with forced diuresis and negative fluid balance. On day 13, almost complete normalization of LV contractility with EF in B-mode up to 60% with slight diffuse hypokinesia was documented (Figure 4).
According to contrast enhanced cardiac magnetic resonance imaging, performed on the 12th day, there were signs of moderate regional fibrosis of a noncoronary nature in the projection of the interventricular septum and LV inferior wall without reliable signs of inflammation activity.
The patient was discharged with improvement and following therapy: sartans, anticoagulants, betablockers, statins.
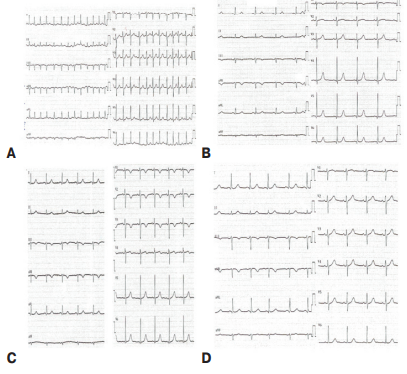
Figure 1. ECG over the time of hospitalization: A) at admission; B) 3 days after electrical cardioversion; C) on 5 day; D) on 12 day.
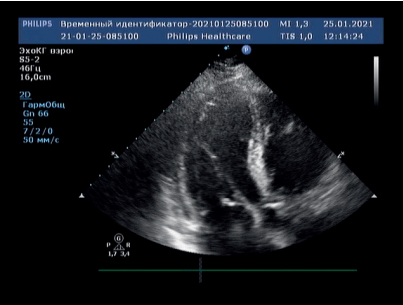
Figure 2. Transthoracic echocardiography on day 3, apical 4-chamber view.
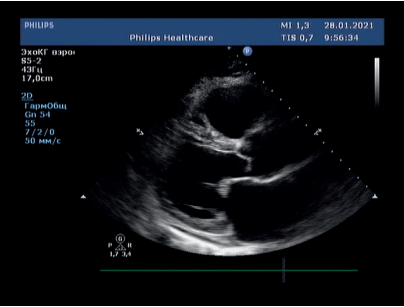
Figure 3. Transthoracic echocardiography on day 6, parasternal long-axis view.
Table 1
Changes of levels of cardiac markers over the period of hospitalization
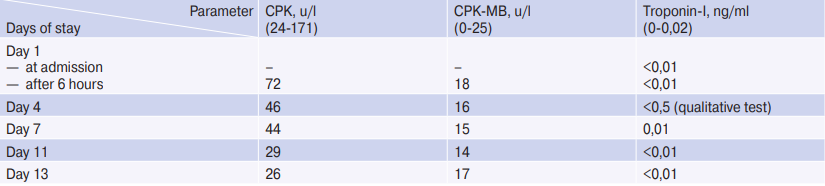
Abbreviation: CPK — creatine phosphokinase.
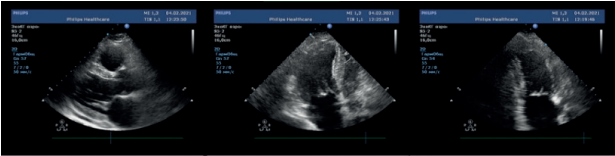
Figure 4. Transthoracic echocardiography on day 13. From left to right: parasternal long-axis view, apical 4-chamber view, apical 2-chamber view.
Discussion
Of course, ACS and myocarditis was considered the possible causes of transient myocardial dysfunction.
In the first case, the patient’s history, typical pain syndrome, and the appearance of T-wave inversion testified in favor of ACS. At the same time, the absence of an increase in cardiac enzymes, significant stenosis according to CAG data, and a rapid recovery of myocardial contractility made it possible to rule out ACS.
Differential diagnosis with myocarditis was based mainly on the identification of hydropericardium, contractility impairment according to echocardiography. However, given the presence of bilateral hydrothorax at the same time, rapid improvement with diuretic therapy, this condition was regarded as heart failure decompensation, the trigger for which was the development of AF episode with treatmentresistant tachysystole. The absence of anamnestic indications of a connection with the infectious process should also be clarified. During the entire stay of the patient in the hospital, none of the analyzes showed an increase in acute phase blood parameters. The final clarification was made by cardiac magnetic resonance imaging, where no data for an acute inflammatory process were obtained.
Decompensated heart failure in this case should be taken as the cause of such pronounced myocardial contractility impairment due to a combination of the identified changes with QT interval prolongation and T wave inversion on the ECG. At the same time, the elimination of congestion when sinus rhythm is achieved against the background of low-dose diuretic therapy is precisely a manifestation of the compensation. However, one should not deny the contribution of tachysystole in AF to the development of a mild systolic dysfunction identified on the eve of hospitalization prior to electrical cardioversion.
In this case report, ruling out the above conditions, we turned to the diagnostic algorithm of takotsubo syndrome (2018). According to the InterTak score [5], which takes into account factors such as female sex, emotional and physical triggers, mental and neurological disorders, the absence of ST segment depression and a prolonged QT interval, the likelihood of takotsubo syndrome in this case is moderate and low (55 points). Referring to the InterTak 2018 criteria, we were able to match the following:
1. Transient local contractility disorders of left or right ventricular walls, which usually do not correspond to the area of blood supply to one coronary artery.
2. Takotsubo syndrome is often (but not always) preceded by a stress trigger (emotional and/or physical).
3. Occurrence of new reversible ECG abnormalities (ST elevation/depression, left bundle branch block, T wave inversion and/or QT prolongation) during the acute phase.
4. No signs of myocarditis.
Criteria such as neurological disorders and pheochromocytoma (considered as a possible trigger), the increase in cardiac markers, as well as the dominant distribution among postmenopausal women did not match in our case. The concentration of brain natriuretic peptide was not determined. At the same time, to definitely attribute the variant of contractility impairment to any of the previously described ones is not possible, since systolic dysfunction was of an atypical nature, debuting from a global decrease in contractility to local hypoakinesia of the apical and anterior septal region, including middle localization. Similar disorders can occur in a typical apical variant, not accompanied by an increase in the contractility of the basal segments. It is important that such a pronounced decrease in myocardial contractility after cardioversion did not match the level of troponins and ECG changes, which often accompanies takotsubo syndrome [6]. The appearance of chest pain during a cycle ergometry as part of myocardial stress scintigraphy with minor coronary stenosis and slowing of coronary blood flow is most likely due to microcirculatory dysfunction, which is important in the development of stress-induced myocardial damage, along with activation of the sympathoadrenal system through the increase in blood levels of catecholamines.
Thus, there is every reason to believe that the patient has takotsubo syndrome, probably caused by electrical cardioversion. Data from a systematic review of cases of takotsubo syndrome, published in 2022, convincingly demonstrate the risk of developing this condition after electrical cardioversion, performed in the vast majority of AF cases (8 cases out of 11), more often within 10 hours. The data obtained during the analysis do not contradict those demonstrated by us in the presented work. At the same time, the role in the development of takotsubo syndrome is determined both for direct damaging electrical effects on the myocardium and for catecholamine-mediated effects [7].
Conclusion
The complexity of pathophysiological mechanisms and the predominance of the role of psychoemotional and physical factors in the development of takotsubo syndrome increase the importance of its timely diagnosis today, given the high and extremely stressful pace of life of the modern generation. The ease of InterTak score use in the prehospital stage and in the initial examination should contribute to its wider use in the early stages of diagnosis. Attention should also be paid to the least common factors in this syndrome (male sex, atypical myocardial dysfunction, etc.), the correct assessment of which will increase the frequency of takotsubo syndrome verification.
Relationships and Activities: none.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Sitkova E.S., Smorgon A.V., Batalov R.E., Andreev A.A., Popov S.V. Takotsubo syndrome in a patient with atrial fibrillation after electrical cardioversion: a case report. Russian Journal of Cardiology. 2022;27(4S):5179. https://doi.org/10.15829/1560-4071-2022-5179
Copy