Association of medical staffing and outcomes in cardiovascular diseases
Prevalence of cardiovascular diseases (CVD) and the need for a highly skilled workforce
Recent decades have seen an increase in life expectancy at birth from 67,2 years in 2000 to 73,5 years in 2019 [1]. This is due to significant advances in the diagnosis and treatment of many diseases, including CVDs. With effective drug therapy and close integration of health care with high technology, CVDs are less fatal but more prevalent. Coronary artery disease (CAD) and stroke have for decades shown the highest disability-adjusted life years (DALYs) and potential contribution to the loss of ‘healthy’ life years in the age groups 50-74 years and over 75 years [2]. CVDs continue to top the list of causes of hospitalization and mortality in the population. In the Russian Federation (RF), high premature mortality from CVDs, which accounts for ~50% of all deaths, is one of the most acute public health problems [3].
The current burden of CVDs on health systems around the world and their projected growth are driving the need to develop human resource capacity and competencies — as factors key to health promotion, accessibility and quality of care (Figure 1) [4]. The cardiac workforce should be understood as a team of professionals working together to implement the principle of continuity of care. However, at the center of the decisionmaking system are cardiologists, who interact with patients at all stages of the CVD continuum and at all stages of care. The widespread use of innovative CVD treatment methods and information and communication technologies sets high requirements for the education, professional competencies and skills of the modern cardiologist.
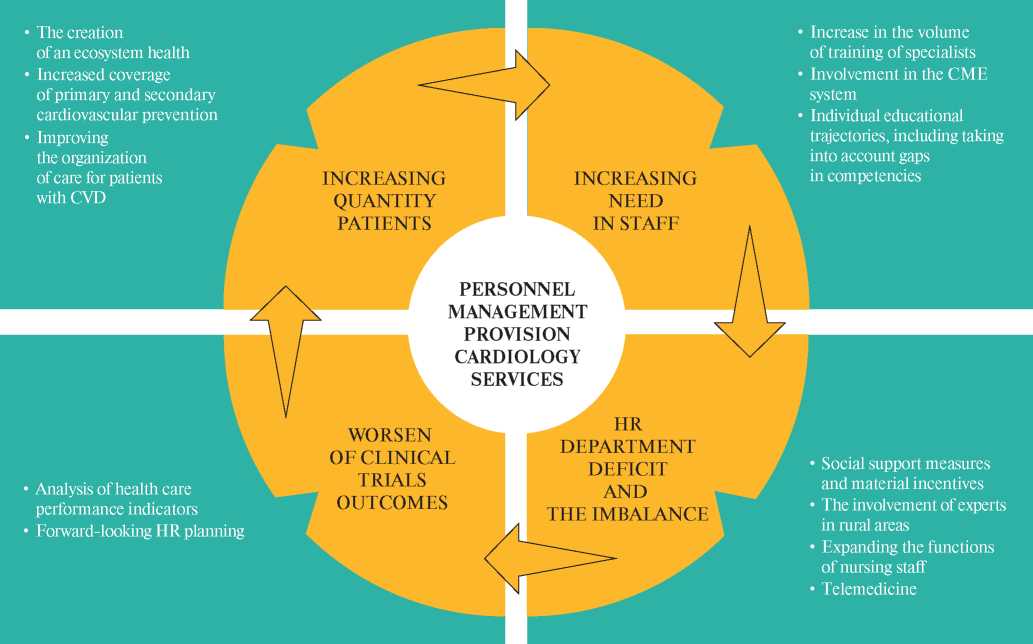
Figure 1. Development of human resource capacity and competencies as factors that play a key role in ensuring access and quality of CVD health care.
Note: the increasing burden of CVDs is the main factor behind the high demand for qualified cardiac professionals and the growing relative and absolute shortage of staff in the system of care for patients with CVDs, which is reflected in the worsening of clinical outcomes in patients with CVDs. Strategies to both increase the number of specialists and improve the quality of their training can improve the efficiency of the whole system of CVD care. Yellow indicates the main challenges for CVD care, while green indicates ways of addressing the identified challenges.
Abbreviations: CVD — cardiovascular disease, CME — continuing medical education.
In order to improve the medical infrastructure and increase the availability and quality of health care and, consequently, to increase life expectancy to 78 years by 2030, the Russian Government approved the national project, the aim of which is reduction of CVD mortality to 450 cases per 100000 people by 2024 [5]. Its achievement largely depends on the availability of qualified specialists in the industry. The shortage or uneven territorial distribution of specialists involved in the provision of health care to patients with CVDs can be critical in the implementation of national objectives. Earlier studies indicate the prognostic value of hospitalization and treatment of CVDs in specialized departments [6, 7], which may be associated with their better equipment, the possibility of more intensive monitoring, timely recognition and treatment of life-threatening complications, more frequent prescription of drugs with proven effects on the quality of life of patients. The present review summarizes the available data on the associations of cardiology staffing indicators and quality of care parameters and outcomes in cardiovascular diseases.
Availability of inpatient cardiologists and in-hospital outcomes for CVDs
In acute or decompensated chronic CVDs, the availability of highly qualified specialists may be a key factor, in addition to the timeliness and profile of hospitalization. A shortage of inpatient cardiologists can potentially lead to delays in life-saving therapy, as well as missed opportunities to improve longterm outcomes — stabilization and correction of significant risk factors, optimal drug therapy and management plans, and patient education.
To assess the potential relationship between inpatient staffing and hospital outcomes, various indicators have been used — the availability and number of cardiologists, the specialist workload in relation to volumes of care per year or the number of contractual patients (Table 1).
Table 1
Studies on the impact of the availability of inpatient cardiologists on outcomes in patients with MI/acute coronary syndrome, HF

Abbreviations: CI — confidence interval, MI — myocardial infarction, HR — hazard ratio, OR — odds ratio, HF — heart failure, CVD — cardiovascular disease.
Table 2
The influence of the specialization of the doctor performing outpatient follow-up on clinical outcomes
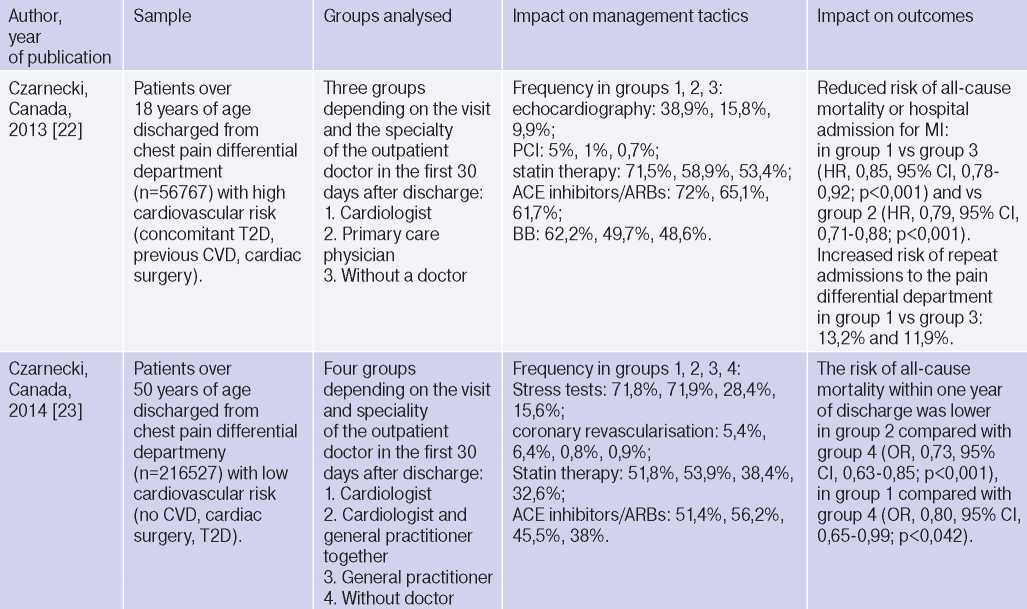
Table 2. Сontinued

Abbreviations: VKA — vitamin K antagonists, BB — beta-blockers, ARB — angiotensin II receptor blockers, CI — confidence interval, ACE — angiotensin-converting enzyme, MI — myocardial infarction, CA — coronary angiography, DOAC — direct oral anticoagulants, HR — hazard ratio, OR — odds ratio, T2D — type 2 diabetes, HF — heart failure, CVD — cardiovascular diseases, AF — atrial fibrillation, PCI — percutaneous coronary intervention, VCR — ventricular contraction rate.
One of the leading causes of hospital admission in CVD patients is decompensated heart failure (HF). According to European studies, 32-44% of HF patients are hospitalized during the year, most of them over 65 years of age [8, 9]. The frequency of rehospitalizations for HF is associated with mortality and inversely correlated with the number of acute care beds in the region [10]. In the analysis of the administrative database of Japan, among patients hospitalized with decompensated HF in hospitals without cardiologists, hospital mortality was significantly higher and adjusted for significant prognostic factors (sex, age, route of hospitalization, HF class, respiratory failure, CAD, hypertension (HTN), atrial fibrillation (AF), life-threatening arrhythmias, renal failure, shock) was 10,7% compared to 5,4%, 7,0% and 7,1% in hospitals with a staff of ?10, 5-9 and 1-4 cardiologists, accordingly [11] .There are significant differences in the practice of managing patients with HF: more frequent prescribing of therapy and therapeutic and diagnostic interventions in hospitals with better provision of cardiologists [11].
Another study demonstrated a 30% reduction in the risk of in-hospital mortality for the population of patients hospitalized with HF in hospitals with the highest ratio of cardiologists to 50 inpatient beds [12]. Dividing all hospitals into quartiles, the group with the highest score (16,7) compared with the lowest (4,4) showed an average 59% increase in the use of beta-blockers, a 38% increase in angiotensin converting enzyme inhibitors and a 27% increase in mineralocorticoid receptor antagonists [12]. Thus, better management of patients with HF by cardiologists may lead to improved hospital outcomes, but also, potentially, by a higher frequency of optimal drug therapy, which reduces mortality, to improved long-term outcomes.
It is noteworthy that better inpatient management by cardiologists compared to non-cardiologists may be associated with a reduced risk of pneumonia, septicemia and urinary tract infection, in addition to improved survival, as demonstrated in a study using propensity score matching depending on age, sex, income level, diagnosis, presence of HTN, type 2 diabetes (T2D), end-stage chronic kidney disease, cirrhosis, hyperlipidaemia, Parkinson’s disease, number of hospital admissions and frequency of emergency department visits [13]. This is particularly important in view of the increasing number of patients with CVD who have non-cardiac disorders at the same time.
Another large national study in Japan (Table 1) has shown that a higher number of cardiologists who are certified as specialists is associated with lower mortality in patients admitted with a wide range of CVDs to an acute care hospital, regardless of equipment, patient demographics and variant of
CVD [14]. However, these associations were more pronounced for smaller hospitals. The emergence of a relative shortage of specialists in large hospitals with an increase in the number of beds and physician workload (high “number of beds per certified cardiologist” ratio) was accompanied by an increase in hospital mortality [14]. In contrast, another study (Medicare, USA, 2004-2006) showed a reduction in 30-day mortality from myocardial infarction (MI) and HF when admitted to hospital with a high annual volume of medical services for these conditions [15]. However, the authors set a volume threshold above which there is no reduction in mortality. These results emphasize that the number of specialists and volumes (which determine specialist experience and are important, particularly in percutaneous coronary intervention and coronary artery bypass grafting [16, 17]) are not the only parameters affecting outcomes. It is not so much the number as the workload of specialists that is fundamental, and this must be taken into account in the territorial planning of specialized health care, the routing of patients with acute CVDs and the rules of interaction between institutions. In particular, a study of the spatial distribution density of cardiologists (the ratio of specialists to the eligible population aged over 65 years) has shown that regions with a low density of cardiologists have higher 30-day and one-year mortality rates in patients with MI (13% and 6%) and HF (19% and 9%) [18].
Outpatient cardiac monitoring and prognosis of cardiovascular patients
A seamless model of management of patients with chronic CVDs, especially elderly and comorbid patients receiving care in different institutions and by different specialists, may reduce CVD mortality [19]. One solution is to establish a cardiovascular risk management system in each region, with continuity between inpatient and outpatient care being an important component of this system [20]. Continuity reduces the number of hospital admissions and the risk of death [21]. Studying the role of the professional managing patients discharged from hospital after an acute cardiovascular event can help to plan and organize the most effective model of follow-up.
Several studies have demonstrated that outpatient follow-up by a cardiologist reduces the risk of adverse events (Table 2). Among high cardiovascular risk patients with a history of T2D, previous MI and/or coronary revascularization, other known CVDs discharged from the differential chest pain unit and presenting within 30 days of discharge to an outpatient cardiologist visit, there was a 15% reduced risk of MI or death compared with patients with a general practitioner visit and a 21% reduction compared with patients without an outpatient visit [22].
These associations were observed, adjusted for a wide range of influencing factors, despite a later visit to the cardiologist (median of 12 (5-20) days after discharge vs 7 (2-15) days for the general practitioner) and a higher proportion of patients with risk factors and previous CVD. For patients in the cardiologist follow-up group, a higher frequency of appointments for diagnostic tests, including stress tests, echocardiography, as well as major classes of cardiovascular drugs and coronary revascularization was found [22]. In a similar analysis of a patient population without diabetes or previous CVD [23], follow-up with a cardiologist together with a primary care physician compared with no visit within 30 days of discharge was associated with a 27% and 19% reduction in risk of death and death or MI, respectively. A cardiologist visit was associated with a tendency to reduce the risk of death by 20% and of death or MI by 13%, whereas no improvement in outcomes was observed with primary care alone versus no follow-up [23]. Patient groups in which the cardiologist was involved in the follow-up were characterized by a higher frequency of use of diagnostic tests, myocardial revascularization and prescription of CAD therapy [23].
Of note, evidence of more frequent adherence to current clinical guidelines, prescription of enhanced screening and optimal drug therapy by cardiologists has been repeatedly confirmed in subgroups of primary and secondary cardiovascular prevention [24], in patients with AF and chronic HF [2528]. A retrospective cohort study including patients with newly diagnosed AF (n=184161, USA) also found an 11% lower risk of death in the first 90 days of follow-up and more frequent prescribing of anticoagulant and antyarrhythmic therapy, statins and angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers [26]. All-cause mortality, as well as stroke and major bleeding rates, were significantly lower among patients with first- diagnosed AF who were followed up for one year by cardiologists compared with patients who did not visit a cardiologist [27]. In another retrospective population-based study of patients with firsttime AF presenting to the emergency department (n=2902, Ontario, Canada), mortality was 32% lower in those with cardiac consultation during the subsequent year of follow-up compared with the group without cardiac consultation. However, there was a higher rate of rehospitalizations with AF, HF and stroke [25]. The study was conducted using propensity score matching, taking into account sex, age, socioeconomic status, cardiologist examination during an emergency department stay and in the 2 years prior to admission, cardioversion, repeat admissions to the emergency department, presence of HF, T2D, stroke, HTN, bleeding, comorbidity, risk of thromboembolic complications by CHA2DS2VASc.
An inverse correlation between the availability of cardiologists per 100 000 population and the frequency of major hospital admissions (r=-0,34, p<0,01) was shown in a large Canadian study, with no relationship between the number of hospital admissions and availability of primary care physicians. However, the availability of cardiologists was also associated with a higher use of different cardiovascular diagnostic tests (relative risk (RR), 1,10, 95% confidence interval (CI), 1,09-1,10, p<0,001), including coronary angiography (RR, 1,03, 95% CI, 1,02-1,04, p<0,001) and echocardiography (RR, 1,16, 95% CI, 1,15-1,17; p<0,001) and noninvasive tests (RR, 1,10, 95% CI, 1,10-1,11; p<0,001) [29]. It is likely that the interpretation of an increased risk of hospital admission with better therapeutic and diagnostic management in cardiology follow-up should not be seen as a negative trend, but rather as an indication of alertness to prevent the development of adverse outcomes.
A particularly complex population of patients with a high risk of adverse outcomes is represented by patients with HF. The Russian RUS-HF study showed better survival during treatment in specialized departments and subsequent follow-up for 3 years after discharge in groups of cardiologists-specialists in HF and cardiologists of the federal center compared to regional center cardiologists (80,3% and 77,9% vs 52%) [28]. It can be expected that in specialized institutions, the outcomes of HF are better due to the participation of a multidisciplinary team in the treatment, technical capabilities, accumulated experience, high professional level of specialists, as well as a greater frequency of prescribing therapy that affects the prognosis [28]. Foreign studies in this area also demonstrate a more frequent use of the main groups of drugs recommended for the treatment of patients with HF, with joint follow-up after discharge of patients hospitalized with HF in the emergency department, by cardiologists and general practitioners, compared with follow-up only by general practitioners or no outpatient follow-up [30].
The reduction in the risk of death associated with the cardiologist’s follow-up after discharge should be interpreted carefully. The very existence of the visit after discharge may reflect several factors such as organizational and related to patient characteristics, greater adherence to treatment and lower severity of the condition. On the other hand, the adjustment for multiple factors that potentially determine the prognosis strongly indicates the presence of a “specialist effect” on improving the quality of health care and prognosis in CVD.
The question of which specialty doctor should observe patients at the outpatient stage, however, cannot be resolved unambiguously. One of the successful areas of personnel policy in the system of care for patients with CVD is the introduction into clinical practice of teams that include nurses with higher education, clinical pharmacologists, and medical assistants. With this approach, a high level of quality of medical services can also be achieved. In particular, a large longitudinal IMPROVE HF cohort study conducted to assess the quality of management of patients with HF or left ventricular dysfunction due to MI at the outpatient stage, which included patients from 162 cardiology practices (n=14891, USA), did not show significant differences in compliance with current clinical recommendations in the groups of patients observed with the participation of medical assistants and nurses and only doctors. In addition, in cardiology practices staffed by medical assistants and nurses with higher education, the training of patients with HF was carried out [31]. In another study of outpatient follow-up of patients after MI by a team or only doctors, there were also no significant differences in mortality within 90 days after discharge (adjusted odds ratio (OR), 1,18, 95% CI, 0,98-1,42), drug treatment (OR, 0,98, 95% CI 0,89-1,08), risk of rehospitalization (OR, 1,11, 95% CI, 0,99-1,26) [32]. At the same time, the patients observed by the team were more likely to suffer from T2D (37% vs 33%), HF (20% vs 16%), were discharged to a medical institution (21% vs 13%), and had more visits during the 90 days of follow-up (median number of visits 6 vs 5) [32].
Availability of cardiologists and mortality from CVD
The results of the research indicate that among a wide range of factors that affect the mortality from CVD, an important role is played by the availability of specialists and availability of qualified specialized healthcare. The prognostic significance of a visit to a specialist has been convincingly demonstrated for patients with chronic diseases (HF, CAD, chronic obstructive pulmonary disease or asthma) living in rural areas. A visit to a specialist, compared to one or more visits to a primary care doctor, was associated with a 15,9% reduction in the incidence of potentially preventable hospitalizations and a 16,6% reduction in death [33].
The relationship between CVD mortality and the number of cardiologists was found in a large epidemiological study conducted using data on the availability of primary care physicians in 3142 US districts from 2005 to 2015. It was found that after adjusting for socio-economic and demographic factors, an increase in the provision of 10 cardiologists per 100 thousand population is associated with a decrease in cardiovascular mortality by 49,4 cases per 1 million population (95% CI, from -76,8 to -22,0 deaths per 1 million population). However, the authors also noted a decrease in cardiovascular mortality by 30,4 cases per 1 million population, with an increase of 10 primary care physicians (95% CI, from -52,4 to -8,4). The obtained results emphasize the significant role of human resources, including the primary health care system, in the outcomes of CVD [34].
In a cross-sectional study of associations between various indicators of the availability of regional health systems and population health indicators in 16 federal states of Germany, an inverse correlation was established between the number of cardiologists and the incidence of CVD [?=-0,689, p=0,031], while no significant associations were found between the availability of general practitioners and endpoints [35]. The total number of residents per 1 department of differential diagnosis of chest pain directly correlated with the incidence of CVD [?=42,730, p=0,036] and related mortality [?=4,962, p=0,002], which can be partially explained by the relative shortage of specialists. The socio-economic characteristics of the federal regions could potentially affect the results, since their impact on mortality rates and demand for medical care has been proven in many studies [36].
Conclusion
Despite the differences in research methodology and indicators analyzed, the observational nature of studies, the possibility of systematic selection errors and underestimation of potentially influencing factors, the results of most studies are consistent and convincingly emphasize the fundamental role of cardiologist in receiving cardiovascular care. The “specialist effect” on cardiovascular outcomes is shown both for different patient populations and different stages of care. The shortage of cardiologists is critical to achieve a sustainable rate of decline in the CVD rate. While the most important elements of an effective HR policy are to ensure that staffing needs are met, that physician shortages in particular specialties are overcome, that geographic disparities are eliminated and that practitioners have a high overall skill level, further research is needed to identify the most appropriate, science-based approaches for strategically choosing a regional HR service and providing it with the right human resources. The development of regionally specific, integrated and tailored solutions to coordinate assistance and provide at least one specialist consultation can save significantly more lives in a shorter timeframe.
