Coronary artery bypass grafting in patients with coronary artery disease and COVID-19: search for an optimal strategy
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first described in early December 2019 and has rapidly spread globally, significantly disrupting healthcare delivery in many countries. The extent of cardiac surgical care also significantly changed due to the redistribution of bedspace resources, which decreased number of cardiac surgery operations around the world. While the measures applied have been beneficial for patients with coronavirus disease 2019 (COVID-19), the implications of postponing elective cardiac surgery for cardiovascular patients need to be considered. It can be assumed that these patients will have progression of the underlying disease, which will increase the number of patients in need of emergency cardiac surgery.
Currently, there are papers where the authors report successful cases of cardiac surgery in COVID19 patients [1][2]. This is a very rewarding experience to understand how cardiac surgery can be adapted to work in a pandemic.
In this article, we want to present our experience in cardiac surgery of patients with coronary artery disease (CAD) and COVID-19 manifested in the early postoperative period after coronary artery bypass grafting (CABG). Given that the incubation period is up to 14 days, it is highly likely that most of these patients had COVID-19 during surgery.
Material and methods
In 2020, 315 patients with CAD underwent elective or emergency CABG (isolated or in combination with treatment of valvular heart disease) in the cardiac surgery department № 11 of V.P. Polyakov Samara Regional Clinical Cardiology Dispensary. In 19 patients, the early postoperative period was complicated by COVID-19 pneumonia. The preoperative characteristics of these patients are presented in Table 1 and some laboratory parameters in Table 2.
Table 1
Preoperative characteristics of patients
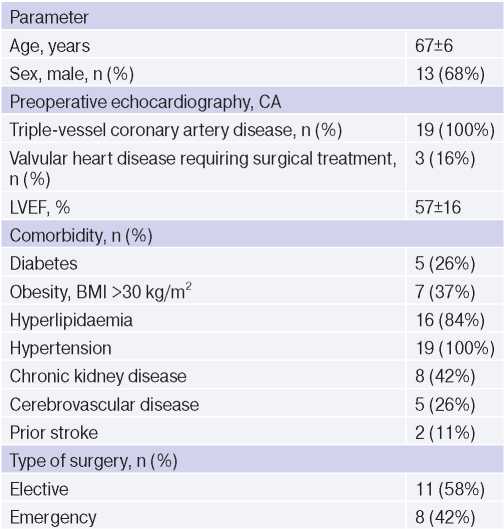
Abbreviations: BMI — body mass index, CA — coronary angiography, LVEF — left ventricular ejection fraction.
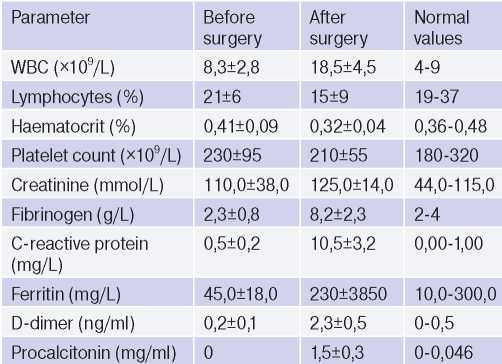
Table 2
Changes in laboratory parameters
All patients participating in our study signed written informed consent. This study was performed in accordance with the Helsinki declaration and Good Clinical Practice standards. The medical ethics committee of V.P. Polyakov Samara Regional Clinical Cardiology Dispensary approved this study.
Statistical analysis. Quantitative variables are presented as mean with standard deviation; categorical variables — as value and its percentage. Descriptive statistics were used to analyse the results.
Results
In the preoperative period, 3-5 days before the procedure, all patients underwent an analysis for identification of SARS-CoV-2 RNA in nasopharyngeal and oropharyngeal swabs by real-time polymerase chain reaction (RT-PCR). All patients were negative for SARS-CoV-2 RNA.
All patients (n=19) with positive SARS-CoV-2 tests in early postoperative period after CABG, operations were performed through a median sternotomy, under cardiopulmonary bypass and blood cardioplegia. In addition to CABG, three patients (16%) underwent treatment of mitral insufficiency. The mean duration of cardiopulmonary bypass was 58,3±11,2 minutes, while the artificial ventilation after surgery lasted 8,3±2,2 hours. No patient had resternotomy for bleeding in the first 24 hours after surgery.
In the early postoperative period (3-5 days), these patients manifested with COVID-19. The following symptoms were common to all patients:
- high-grade fever, poorly treated with standard antipyretics;
- general weakness, more pronounced than in patients after CABG without COVID-19;
- severe shortness of breath;
- moderate (92-95%) to severe (<90%) decrease in blood oxygen.
According to chest X-ray, only one patient (on the 4th day after surgery) was diagnosed with double pneumonia, while other patients (on the 3-5th day after surgery) had normal chest X-ray performance.
According to chest computed tomography (CT), all patients had a picture of single or double multisegmental pneumonia in the form of ground-glass opacity areas. The lesion area of lungs varied from 10% to 55% (Figures 1, 2).
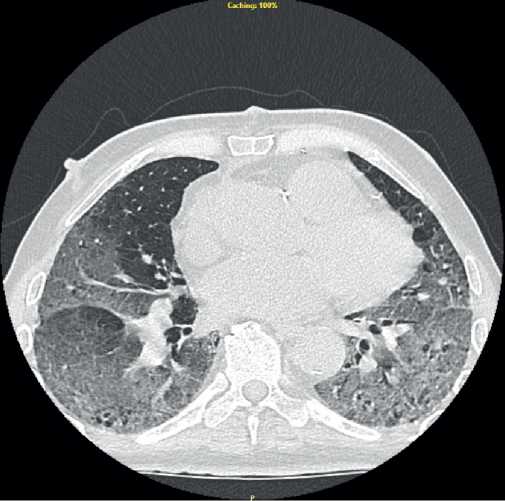
Figure 1. Chest CT scan of the patient 4 days after CABG with signs of pneumonia.
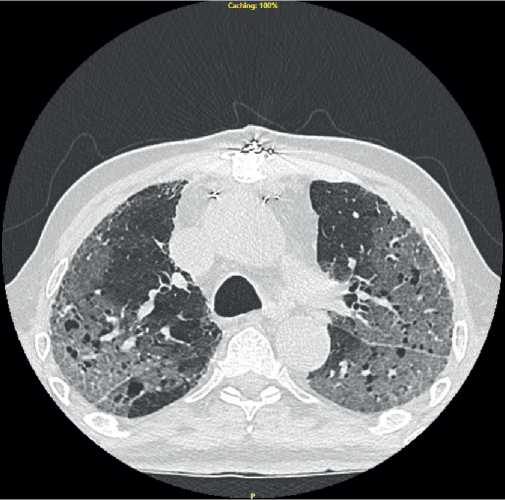
Figure 2. Chest CT scan of the patient 5 days after CABG with signs of pneumonia.
In all patients, according to laboratory tests, an increase in the level of fibrinogen, ferritin, procalcitonin, C-reactive protein and D-dimer was noted (Table 2).
After suspicions of COVID-19, the patients were re-analysed for SARS-CoV-2 RNA in nasopharyngeal and oropharyngeal swabs using real-time RT-PCR and 11 (57,8%) patients were positive.
Patients with suspected COVID-19 were sequestered in an isolation ward. Conservative treatment was carried out in accordance with Russian Ministry of Health guidelines [3]. All patients were transferred to infectious diseases hospitals within 24 hours after detection of pneumonia using CT.
Sixteen patients transferred to infectious diseases hospitals were subsequently discharged from hospitals in a satisfactory condition on days 14-17 after transfer. Three patients died from various COVID-19 complications in the next 7-10 days (mortality rate, 16%). Two of them, 65- and 72-year-old men, who underwent elective isolated CABG, did not have severe comorbidities. The third deceased patient, a 76-year-old woman, underwent a combined operation — CABG and mitral valve repair. Among the comorbidities, the woman had class I obesity, stage IIIB chronic kidney disease, type II diabetes.
Discussion
The COVID-19 pandemic has led to a significant decrease in extent of elective cardiac surgery world-wide. In addition, cardiologists and cardiac surgeons faced the need to solve a serious problem: the risks arising from postponing surgery in cardiovascular patients should be correlated with the risks of performing surgery during the incubation period or the hospital-acquired COVID-19.
Currently, there are few data on surgical treatment outcomes in patients with COVID-19. Lei S, et al. reported the treatment outcomes of 34 patients who underwent various operations during the COVID-19 incubation period. The authors suggested that surgery may worsen the progression of disease, since the mortality rate among these patients was 20,6% (higher than in surgical patients without COVID-19) [4]. The international multicenter cohort COVIDSurg Collaborative study with 1128 patients with confirmed COVID-19 who underwent a wide range of operations, the 30-day mortality rate was 23,8%, which is also higher compared to patients without COVID-19 [5].
Rescigno G, et al. [6] presented the outcome of emergency CABG surgery in an asymptomatic patient who died in the early postoperative period due to COVID-19 related pulmonary complications. The authors acknowledge that an undiagnosed infection may have caused a refractory pathological response after cardiac surgery. Indeed, recent studies have suggested that COVID-19 patients are at a higher risk of thromboembolism. In addition, there is a consensus that SARS-CoV-2 has a direct adverse effect on the myocardium due to the high expression of angiotensin-converting enzyme 2 [7].
Thus, the available data assume that cardiac surgery patients are the most vulnerable cohort of patients who have worse outcomes in the presence of concurrent COVID-19. This is also confirmed by our results of cardiac surgery treatment of patients in the incubation period of COVID-19. Mortality after CABG among these patients was 16%, while the average mortality worldwide in this category of patients is ~1%.
At the same time, a number of authors reported relatively satisfactory outcomes of CABG in patients during the incubation period of COVID-19, as well as in height of disease [1][2]. The analysis of these works is necessary to develop a certain strategy for the management of cardiac patients in the context of COVID-19 pandemic.
The outcomes of CABG obtained by us and foreign authors in patients with CAD and COVID-19 allow to single out following recommendations:
1. All patients indicated for cardiac surgery should undergo a full preoperative examination, after which, a multidisciplinary team of specialists (Heart Team) should assess the urgency of surgery;
2. To reduce the risk of hospital-acquired COVID-19, patients should be in the hospital for as little time as possible before the operation, and after procedure, it is necessary to minimize the number of patient contacts with others;
3. Routine testing for SARS-CoV-2 should undergo all patients preparing for surgery to identify asymptomatic and subclinical disease;
4. Considering that the sensitivity of RT-PCR for SARS-CoV-2 RNA in nasopharyngeal swab is <70% (according to some data, 30-40%), it is necessary to analyse the level of laboratory infection markers (C-reactive protein, ferritin, procalcitonin, fibrinogen, D-dimer), as well as data from additional diagnostic tests, such as measuring the blood oxygen saturation, and in doubtful situations — chest CT;
5. Any clinical change suspecting COVID-19 in the perioperative period is an indication for additional RT-PCR and chest CT (chest CT has a higher sensitivity (98%) than RT-PCR to determine the COVID-19);
6. When COVID-19 is confirmed, it is necessary to start treatment as soon as possible in accordance with current guidelines.
Conclusion
Despite the COVID-19 pandemic, it is necessary to continue to provide cardiac surgery for cardiovascular patients. The development of new screening strategies, standard guidelines and protocols for the management of cardiac surgery patients in a pandemic will contribute to an earlier detection of COVID-19 and, accordingly, a timely change in treatment strategy.
