Coronavirus disease 2019 in a patient with CADASIL syndrome: a case report
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is a rare genetic disorder with autosomal dominant inheritance caused by a mutation in NOTCH-3 gene, located on the 19p13 chromosome. This disease is characterized by a low prevalence: there are 2-5 cases per 100 thousand people worldwide; however, its incidence in different populations may differ [1].
Clinically, CADASIL syndrome is most often manifested by recurrent ischemic episodes leading to dementia, gait abnormalities, urinary incontinence, pseudobulbar palsy, migraine (with and without aura), and epileptic seizures. Migraine with aura is an early characteristic feature of CADASIL, occurring in 20-50% of patients with an average age of 30 years. Transient ischemic attacks and lacunar strokes in CADASIL occur in 60-85% of patients aged 50-60 years. Cognitive impairment is often an early manifestation of CADASIL syndrome. Epileptic seizures develop in 5-10% of patients [2].
The coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) poses a serious threat to humanity and is associated with a wide range of clinical respiratory syndromes ranging from mild upper respiratory tract symptoms to life-threatening progressive viral pneumonia [3]. Patients with severe COVID-19 are characterized by respiratory failure and progressive hypoxemia, which often require respiratory support. Chest computed tomography (CT) in patients with COVID-19 reveals numerous ground glass opacities, predominantly round, of varying length with or without consolidation, which meet Berlin criteria for acute respiratory distress syndrome [4]. The hallmarks of COVID- 19 include vascular disease caused by endothelial dysfunction and other factors. COVID-19 is also characterized by coagulopathy, which manifested by skin abnormalities, indicating thrombotic microangiopathy, as well as diffuse alveolar damage due to fibrin thrombi formation; laboratory changes in these patients are characterized by increased levels of D-dimer and ferritin [5].
Much of our knowledge regarding strokes associated with SARS-Cov-2 or those aggravated by a viral infection is based on data from a series of single-center cases, and there are no clear algorithms for treating these patients. Efforts are under way to improve diagnosis, risk factors and treatment approaches in patients with COVID-19-related strokes.
We present a case report of a patient with CADASIL syndrome and moderate COVID- 19 — a combination of congenital and infectious angiopathies.
Case report
Female patient aged 56 years was admitted to the infectious diseases’ hospital with a previously identified CADASIL syndrome, confirmed COVID- 19, and bilateral viral multisegmented pneumonia. Upon admission, the patient complained about severe weakness and low-grade fever.
Medical history. It is known that since 2010 memory loss and gait abnormalities have appeared. Since 2010, sensory aphasia, motor apraxia, impaired right-left orientation, finger agnosia, pseudobulbar palsy, bilateral pyramidal insufficiency, mild bilateral cerebellar ataxia have been diagnosed. In 2015, at the Research Centre for Medical Genetics in Moscow, she was examined for mutations in the NOTCH3 gene (CADASIL Syndrome). The heterozygous mutation c.548G> T (p.Cys183Phe) was revealed, which confirmed a CADASIL. Subsequent admissions to the neurological clinic showed progression of neurological symptoms, increasing cognitive impairment (Montreal Cognitive Assessment score of 21, Mini-Mental State Exam score of 17, Frontal Assessment Battery of 6). Severe cognitive impairments were diagnosed in 2020 (frontal- subcortical dementia). Duplex ultrasound of the brachiocephalic arteries revealed no atherosclerotic plaques and no intima-media thickening (Figure 1). In 2019, electroencephalography revealed abnormalities within the disorganized type. There was no epileptiform activity.
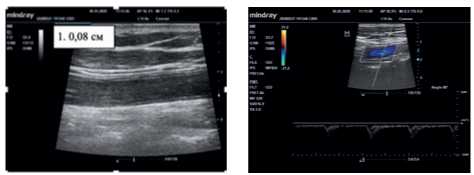
Figure 1. Carotid ultrasound.
Note: common carotid artery, internal carotid artery, and external carotid artery are patent throughout; diameters are sufficient; velocity parameters are within normal limits (in the common carotid artery, the blood flow rate was 80,0 cm/sec, external carotid artery — 48,0 cm/sec; internal carotid artery — 42,0 cm/sec). The intima-media thickness was 0,08 cm.
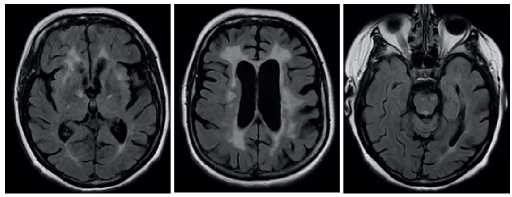
Figure 2. Brain MRI.
Note: MRI picture of multiple focal discirculatory abnormalities in the brain; numerous post-ischemic lacunar cysts, periventricular areas of leukoaraiosis; expansion of CSF spaces.
Using polymerase chain reaction, Herpes and Borrelia were not revealed in cerebrospinal fluid (CSF) and blood. Any rheumatic disease and antiphospholipid syndrome were not revealed. Oligoclonal IgG bands in serum and CSF was not revealed, while free light chains, kappa and lambda in serum and CSF were not elevated. Myelin basic protein and anti-aquaporin antibodies were in normal range. Analysis for HW, HBsAg, HCVAb, RW in CSF and blood were negative.
With regular courses of neurometabolic therapy, irregular intake of NMDA receptor antagonists and acetylcholinesterase inhibitors, no significant positive dynamics was observed. Since 2019, the patient has been receiving continuous therapy: perindopril (5 mg) + indapamide (1,25 mg); atorvastatin (10 mg); metformin (850 mg); akatinol memantine (10 mg); levetiracetam (500 mg).
Development of COVID-19. Seven-eight days before hospitalization, the patient developed weakness, decreased appetite, cognitive impairment, and low- grade fever. At admission to the infectious diseases’ hospital, moderately grave condition was noted. Temperature of 38,0° C. Pulse: 97 bpm, rhythmic, satisfactory filling, symmetrical. Blood pressure: 115/70 mm Hg. Respiration: spontaneous, efficient, rhythmic. Respiratory rate of 21 breaths per minute and SpO2 92% were recorded. Patient communication was significantly limited due to dementia. It was impossible to assess the patient’s sense of smell, eye movements, visual fields, and sensitivity. Pupils D=S. Slow photoreaction was noted. Convergence was not appreciated. End-position nystagmus with extreme abduction of the eyeballs was revealed. Corneal reflexes were preserved. Trigeminal neuralgia was not detected. Swallowing was not disturbed. Reduced pharyngeal reflexes and dysarthria were determined. Symptoms of oral automatism were caused. The palmar grasp reflex on the right was revealed. Upper limb muscle tone was increased in a pyramidal pattern. Diffuse muscle wasting. Muscle strength cannot be reliably assessed due to cognitive deficit. Brisk biceps and knee reflexes, D>S; triceps, carporadial, Achilles reflexes, D=S. Abdominal reflexes were preserved. Bilateral Babinski reflex was presented. Pain response was preserved on both sides. Coordination tests could not be assessed. Meningeal signs were not revealed.
Thus, the following syndromes were identified: cognitive impairment (frontal-subcortical dementia), pseudobulbar, sensorimotor aphasia, bilateral pyramidal insufficiency, pelvic organ dysfunction of central origin, indicating a multifocal vascular process.
According to magnetic resonance imaging (MRI), a picture of multiple focal discirculatory abnormalities in the brain; numerous post-ischemic lacunar cysts, periventricular areas of leukoaraiosis. Expansion of CSF spaces (Figure 2).
According to chest computed tomography (CT) at admission, grade 2 bilateral viral pneumonia was revealed. The English National Early Warning Score (NEWS) of 6 was detected. Decompensated alkalosis (Ph, 7,600) was noted, as well as a decrease in oxygen partial pressure to 53,0 mm Hg (Table 1). Grade 1 respiratory failure was diagnosed. The blood tests showed a high level of C-reactive protein (CRP), a slight increase in fibrinogen and D-dimer levels. White blood cell count and procalcitonin level were within the normal range (Tables 2, 3).
Table 1
Changes in haematological parameters

Abbreviations: GFR — glomerular filtration rate, RBC — red blood cells, WBC — white blood cells.
Table 2
Arterial blood gas changes
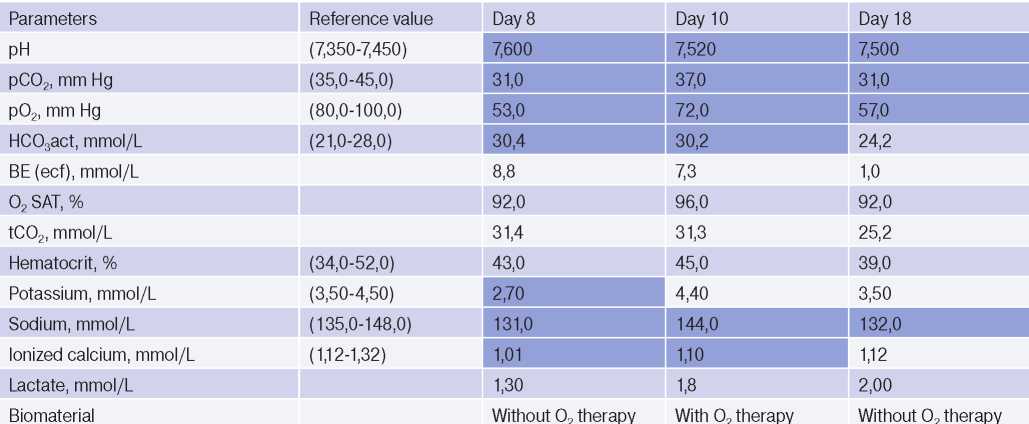
Table 3
Changes of serum CRP concentration
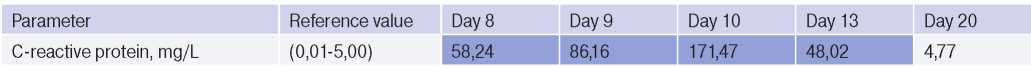
On the 11th day of illness, the maximum level of CRP (171,47 mg/L) was noted. Chest CT scan revealed glass opacities with multiple foci consolidation (both in the peripheral and central peribronchial areas) and pronounced reticular changes (with predominant localization in the dorsal and dorsal-basal parts). The extent of the lung tissue damage was 65-70%. The high probability of COVID-19 was detected. CT scan meet the criterial for grade 2-3 pneumonia. When compared with previous image, there was a negative trend.
According to the current temporary guidelines for the prevention, diagnosis and treatment of COVID- 19, therapy with hydroxychloroquine in combination with azithromycin (hydroxychloroquine 400 mg twice a day, then 200 mg 2 twice a day within 6 days + azithromycin 500 mg 1 time per day for 7 days) is indicated. Taking into account the severe neurological deficit, persistence of fever and the need for oxygen support, an increase in CRP levels and negative dynamics in chest CT, it was decided to abandon this treatment regimen in favor of glucocorticoid drugs. After 10 days of dexamethasone therapy (12 mg per day for 10 days, 8 mg per day for 11 days, 4 mg per day for 12 days, followed by withdrawal of glucocorticoids), the fever was stopped, the CRP level normalized, and the neurological status improved as a slight regression of cognitive impairments — the comprehension of addressed speech improved. An improvement was also noted in fixing the hammer in the horizontal direction. With the abolition of oxygen support, the increase in lactate level was not observed, which indicated the absence of significant tissue hypoxia (Table 2). According to chest CT image, in the peripheral and central parts of both lungs, lobular merging and multilobular areas of glass opacities with indistinct contours were preserved. Similar nodular compaction in the right upper lobe was identified. Transformation of some interstitial infiltrates into perilobular reticular compactions, parapleural and peribronchovascular areas of consolidation with cordlike contours was determined predominantly in the dorsal-basal areas of both lungs. The extent of lung changes decreased in comparison with previous CT image (Figure 3).
Taking into account the high risk of intravascular thrombosis, the patient received therapy with low molecular weight heparins (enoxaparin sodium) at a therapeutic dose of 1 mg/kg from the first day of hospitalization (bleeding risk was determined using the HAS-BLED score). The effectiveness of anticoagulant therapy was assessed by CT cerebral and chest angiography at the peak of CRP concentration. According to head and neck CT angiography, data suggestive of stenosis/thrombosis were not obtained (Figure 4). No CT signs of thromboembolism of the major and intermediate pulmonary artery branches were obtained.

Figure 3. Changes of chest CT on the 8th, 14th and 21st days of a viral infection.
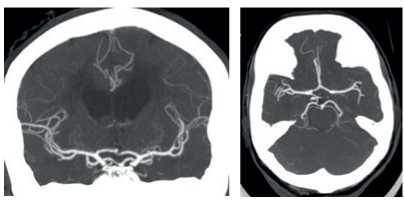
Figure 4. Head and neck CT angiography.
Note: carotid artery diameter was not altered; no contrasting defects; no pathological tortuosity. The vertebral arteries typically depart, enter the C6 transverse foramen, passable, not narrowed, the left one is dominant. Intracranial segments of the internal carotid arteries, basilar and cerebral arteries are passable, not narrowed. The anterior communicating and right posterior communicating arteries are well developed. The left posterior communicating artery is not developed. There is a diffuse expansion of brain ventricles and decrease in periventricular white matter density.
Discussion
COVID-19 is a novel disease caused by the SARS-CoV-2 virus, characterized by fever, cough, myalgia and eventually shortness of breath. Despite the characteristic manifestation of COVID-19, atypical symptoms such as gastrointestinal distress and neurological symptoms, including headache, altered mental status, anosmia and seizures, are common. Often, severe patients with COVID- 19 develop cardiovascular complications, such as myocardial infarction, stroke, but the relationship between infection and these complications is complex and poorly understood. Herpes viruses, such as the varicella-zoster virus, have been shown to invade the vessel wall, causing cerebral vasculopathy. In comparison, Cytomegalovirus, Chlamydia pneumonie, and other pathogenic organisms are closely associated with atherogenesis and plaque instability. In addition, recent bacterial or viral infections are known to temporarily exacerbate pre-existing vascular risk factors for stroke [6]. Various COVID-19 reviews have suggested that infection create an inflammatory environment that predisposes to stroke by activating prothrombotic pathways that affect plaque stability, causing endothelial dysfunction, intimal thickening, leading to arterial wall remodelling. In COVID-19 patients, strokes are usually associated with the activation of the renin-angiotensin system, procoagulation, and massive release of inflammatory cytokines (cytokine release syndrome) [7].
Strokes in CADASIL patients tend to damage subcortical structures. Brainstem involvement is much less common [8]. Interestingly, studies on animals have shown that coronaviruses may have tropism to the brainstem. At the same time, previously conducted studies with a group of coronaviruses in preclinical models showed that when coronaviruses penetrate into the brain, the mortality rate in animals increases, which is presumably due to dysfunction of cardiovascular centre in the brainstem [9]. Our patient had risk factors for vascular disease: obesity, hypertension and CADASIL
The patient’s hypertension was controlled within the optimal range, and the CADASIL-related brain abnormalities according to MRI remained stable over the years, as did the neurological symptoms. It is possible that SARS-Cov-2 infection could have contributed to the deterioration of CADASIL course — aggravation of neurological symptoms and cognitive functions. It should be noted that with timely treatment, the patient had a reduced risk of spontaneous thrombosis — D-dimer levels were within normal limits, while the blood concentration of C-reactive protein during glucocorticoid therapy quickly normalized. Treatment with low-molecular-weight heparins in therapeutic dosages was also carried out. Neurological and cognitive impairments were temporary and most likely associated with viral intoxication.
Thus, in patients with a combination of congenital and infectious angiopathies and COVID-19, neuroimaging is necessary to rule out new foci of cerebrovascular disturbance. It is recommended that early initiation of direct anticoagulant therapy may be beneficial in reducing the thromboembolism risk in these patients. In the presence of respiratory failure and depending on the severity of patients with CADASIL and COVID-19, oxygen therapy is recommended to reduce hypoxia, which also affects the progression of neurological symptoms. Such patients are indicated for invasive and non-invasive mechanical ventilation, continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP) therapy or high-flow nasal cannula oxygen in patients of moderate severity. The appointment of a specific antiviral treatment is controversial. The appointment of therapy should be carried out in accordance with the COVID-19 guidelines of the Ministry of Health of Russia [10].
