Comparison of open femoral exposure and percutaneous access in endovascular reconstruction of the thoracic aorta: a two-center retrospective study
Аннотация
Aim. To analyze the efficacy and safety of the percutaneous transfemoral puncture technique for TEVAR (thoracis endovascular aortic repair).
Material and methods. The retrospective study included 89 patients with aortic pathologies, for whom endovascular repair was performed: 51 patients (57%) with aortic dissection (type I DeBakey — 30 cases (58,8%) and type III — 21 (41,2%)), 38 (43%) patients with aortic aneurism. 82% of patients were male, the median age was 57 years (minimum age 17 years, maximum age 75 years). All patients were divided into two groups: in the first group (48 patients) endovascular aortic repair was performed under endotracheal anesthesia with open femoral exposure of the common femoral artery (CFA), in the second group (41 patients) — by percutaneous puncture method under local anesthesia. Technical and clinical aspects of procedures were analyzed.
Results. Technical success of endovascular repair was achieved in 100% cases in both groups. The duration of the operation in the group with percutaneous access was statically significantly shorter (120 (94-150) minutes vs 87(60-120) minutes, p=0,001). Also, the time spent by patients in the intensive care unit and the period of hospitalization (18 (14-22) hours versus 1 (0-3) hours, p=0,001; 5 (4-6) days versus 4 (3-5) days, p=0,03) was shorter. In the open access group 2 (4,2%) patients developed access-related complications – acute thrombosis of the common femoral artery and hematoma of the postoperative wound, which required additional surgical aid – thrombectomy from the CFA, the second patient had evacuation of the hematoma of the postoperative wound. Cite-related complications in the second group were not observed. No major complications including neurological deficits and hospital mortality were observed in both groups.
Conclusions. Thoracic endovascular aortic repair (TEVAR) using percutaneous access under local anesthesia in stable patients has proven to be safe and effective. The operation time is significantly reduced and this approach in most cases eliminates the need for the patient to stay in the intensive care unit in the early postoperative period. Possibility of early mobilization of the patient appears with reducing of the duration of hospitalization.
Endovascular techniques have revolutionized the treatment of patients with various aortic pathologies, but despite significant technical progress in the manufacture of instruments, stent-graft delivery systems have a large diameter from 18F to 26F, which requires adequate access to the common femoral artery (CFA) and can be considered as a limiting factor for the percutaneous method [1-3]. For this reason, at the present stage, a number of centers prefer open surgical access. However, the open arteriotomy can lead to a number of serious complications such as formation of hematoma, lymphoma, seroma, lymphocele, postoperative scar and wound infection that results in the necessity of additional interventions and increasing the time of hospitalization of patients [4][5].
The appearance on the market devices for percutaneous puncture suturing the arterial wall has made a revolution in the endovascular aortic reconstruction. The use of the Perclose Proglide (Abbott Vascular, Redwood City, CA, USA) devices is an important step in reducing the invasiveness of the procedure. Increasingly, the specialized literature gives examples of routine use of such devices. Unfortunately, many of them are not registered on the domestic market. Some authors note that in a number of clinics this technique is a full-fledged alternative to surgical isolation of the femoral artery [6]. Moreover, this group of patients is generally more satisfied with the treatment process due to reducing the time of the operation and the length of stay in the clinic [7][8]. The use of local anesthesia for the puncture access contributes to not only early diagnostics of the neurological disorders such as ischemia of the spinal cord and brain, but also generally reduces the invasiveness of the procedure. During the process of endoprosthesis delivery, the aortic wall undergoes significant pressure, especially pronounced in the isthmus area. This may cause the discomfort which warns the surgeon about the danger of rupture or retrograde dissection of the aorta. A patient under general endotracheal anesthesia cannot inform about these senses [9][10]. The study is aimed to compare the open and puncture access in endovascular reconstruction of thoracic aorta.
Material and methods
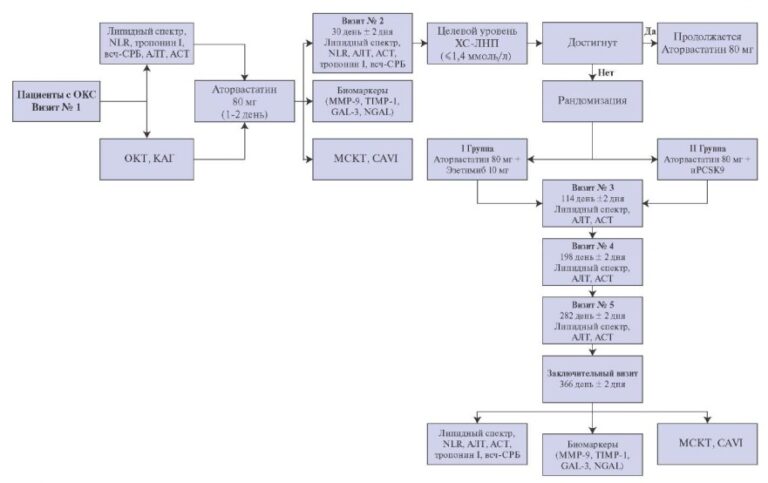
We made the retrospective analysis of the nineyear work experience of the Federal State Budgetary Institution “Federal Center for Cardiovascular Surgery” of the Ministry of Health of the Russian Federation (Astrakhan) and the Bashkir State Medical University for the period from 2012 to 2021. The study included the patients with aneurysm and dissection of thoracic aorta. The patients in acute phase of the pathological process and the patients treated with endovascular techniques were excluded. The total number of the included patients was 89, and 82% of them were men (73 patients). The median age was 57 years (the minimum age was 17 years, and the maximum was 75 years). Endoprosthetic repair of thoracic aorta aneurysms was performed in 38 patients (43%), thoracic aorta dissection — in 51 patients (57%). De Beiki type I was recorded in 30 cases (58,8%), III type — in 21 cases (41,2%). Stanford type А — 31 cases (61%), type В — 20 cases (39%).
The study includes two groups of patients. The first group includes 48 patients — aortic stent-graft implantation was performed under general endotracheal anesthesia and with traditional isolation of CFA. The second group includes 41 patients — the local anesthesia and percutaneous puncture method of endoprosthesis delivery were used.
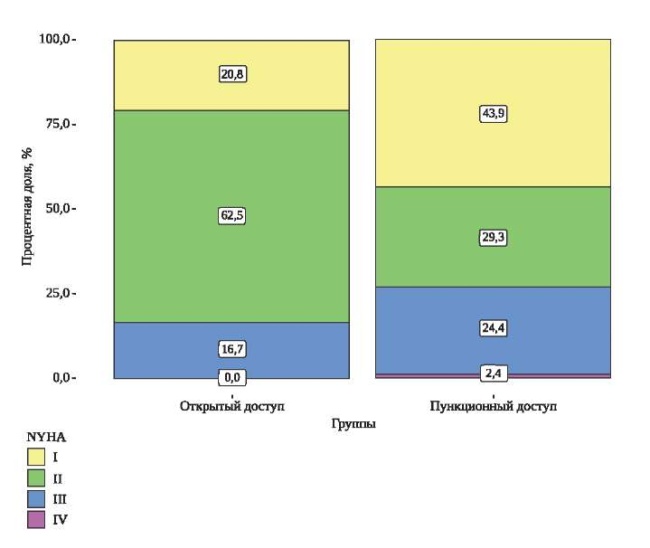
These groups did not differ from each other in main demographic parameters and concomitant diseases (Table 1, Figures 1 and 2). More frequently, the puncture method was used in patients of more elderly age: the median age in the group with the open access was 56 years (46-61), while in the group with the percutaneous puncture method — 62 years (53-69), р=0,01. Because of small size sample we decided to refuse the conduction of propensity score matching and to perform the retrospective analysis despite of statistically significant difference in age. Severe heart failure of functional class III-IV according to New York Heart Association (NYHA) was met in both groups without a statistically significant difference (in 8 patients of the 1 group (16,7%) and in 10 patients of the 2 group (24,4%), р=0,4).
Table 1
General characteristics of the patients included in the study

Abbreviations: AH — arterail hypertension, ACVA — acute cerebrovascular accident, CBS — coronary bypass surgery, CKD — chronic kidney disease, COPD — chronic obstructive pulmonary disease, FC — functional class, IHD — ischemic heart disease, NYHA — New York Heart Association, PCI — percutaneous coronary intervention.

Figure 1. The age of patients included in the study, depending on the access.

Figure 2. The analysis of the functional class parameter according to NYHA depending on the access.
Technical aspects of interventions. To treat patients in both groups, the Medtronic & Ankura`s stentgrafts Valiant Captivia of Lifetech company were used. The diameter of the delivery device is 22-25F. The morphology of the vessels was precisely analyzed by contrast-enhanced multispiral computed tomography. In the group with open access, endoprosthetic repair of aorta was performed under general endotracheal anesthesia with surgical isolation of CFA. In the group with percutaneous puncture access, the endoprosthetic repair of aorta was performed under local anesthesia. The local anesthesia was performed by pricking the puncture site with 0,25% — 20 ml of lidocaine solution. If the adequate local anesthesia was not achieved, intravenous bolus or continuous administration of 0,005% — 1,0-2,0 ml of fentanyl solution in dilution with NaCl was added. In puncture access, the suturing of the artery was performed using two Perclose Proglide (Abbott Vascular, Redwood City, CA, USA) devices according to adopted technique: after performing the puncture of the artery according to Seldinger technique and installing the introducer 6F, the suturing was performed by the two devices alternately (with angulation of the suturing systems at 90? relatively to each other) followed by re-installation of the introducer and further entry of rigid conduction and implantation of stent-graft. There were no conversions with transition to general endotracheal anesthesia and open access. During entire operation all the patients were conscious, and neurological monitoring for timely diagnostics of intraoperative circulatory disorders of the brain and spinal cord was continuously conducted.
Intraoperative angiography of the arteries of the lower extremities on the side of access was performed. In the postoperative period, all patients underwent puncture site monitoring and duplex ultrasound examination of the inguinal region and retroperitoneal space for early diagnostics of retroperitoneal hematoma.
Statistical analysis. The statistical analysis of the material was performed using a software package IBM SPSS Statistics 26 (Chicago, IL, USA), Jamovi (Version 1.6.9) (Computer Software). We verified all quantitative variables for the type of distribution using the Shapiro-Wilk criterion because the number of patients in both groups was <50. The quantitative parameters having a normal distribution were described using arithmetic means (M) and standard deviations (SD), the limits of the 95% confidence interval (95% CI). In case of the absence of a normal distribution, we described the quantitative data using the median (Me) and the lower and upper quartiles (Q1-Q3). The categorical data were described with absolute values (n) and percentages (%). The comparison of the two groups by a quantitative parameter having a normal distribution with unequal dispersions was performed using the Welch t-test. The comparison of the two groups by a quantitative parameter, the distribution of which differed from the normal one, was performed using the MannWhitney U test. The comparison of percentages in the analysis of four-field conjugacy tables was performed using Pearson’s chi-squared test (with values of the expected phenomenon >10) and Fisher’s exact test (with values of the expected phenomenon <10). The comparison of percentages in the analysis of multipole conjugacy tables was performed using Pearson’s chi-square test. The critical significance level when checking statistical hypotheses was taken as 0,05.
Results
The technical success of the stent-graft implantation was achieved in 100% of cases in the investigated groups. The duration of the operation in the group with puncture access was statistically significant shorter (120 (94-150) min vs 87 (60-120) min, р=0,001). We recorded the reduction of the time spent by the patients in the intensive care unit (18 (14-22) hours vs 1 (0-3) hours, р=0,001); this led to a significant reduction of the overall hospitalization period (5 (4-6) days vs 4 (3-5), р=0,03). 2 (4,2%) patients in the first group had the accessassociated complications — acute CFA thrombosis and postoperative wound hematoma that required the additional surgical manipulations — thrombectomy from CFA and evacuation of postoperative wound hematoma, respectively. There were no such complications requiring a surgical intervention in postoperative period in the second group. In 3 cases (7,3%), we observed unsatisfactory hemostasis directly after suturing by two Perclose Proglide systems, that required the use of additional closure device Angioseal 8F (Terumo). We did not find a statistically significant difference between the groups in the occurrence of complications depending on the access. There were none of cases of the neurological deficit occurrence. The hospital lethality rate was 0 in both groups.
The intra- and postoperative data were shown in Table 2 and in Figures 3 and 4.
Table 2
Intraoperative and postoperative parameters

Abbreviation: ICU — intensive care unit.

Figure 3. Duration of the operation depending on the access.

Figure 4. Time spent in the intensive care unit depending on the access.
Abbreviation: ICU — intensive care unit.
Discussion
The extension of indications for the use of percutaneous puncture access for large-caliber delivery devices does not lead to an increase in the number of access-associated complications, while maintaining the maximal technical success of the entire procedure. With the accumulation of experience with suturing devices in our clinics, the tactics for their use have been changed — we actively use a combination of devices with a different mechanism for the closure of an arterial defect. Currently, one system is always used first: Perclose Proglide. At the end of the operation, after tightening the node, the quality of hemostasis is evaluated. In case of major bleeding, we additionally use the second Perclose Proglide device. If the leakage from the puncture site remains, we add hemostasis by using the Angioseal 8F device. In the absence of such a device, it is acceptable to perform prolonged manual compression until complete hemostasis is achieved, that is actively used in a number of centers. In our opinion, the use of an additional device for complete hemostasis is the most reliable and allows you to confidently prevent bleeding in the postoperative period, especially when the patient begins to get up and move around. It should be noted that in our center, we use one suturing device while working with the instruments of no more than the 16F caliber. The importance to explore the effectiveness and safety of the use of number and types of suturing devices is caused by not only accumulation of the experience of the use but also by the appearance of new hemostasis systems and progressive decrease in the diameter of endovascular instrument delivery systems.
Monitoring the results of aortic prosthetic repair using the puncture access, exactly the obtaining a reliable reduction of the time spent by patients in the intensive care unit, led to a change in approaches to postoperative logistics. For instance, currently, after the operation, the patients are transferred immediately to the surgical ward, bypassing the intensive care unit, which is safer, more comfortable for patients and brings economic benefits for the clinic.
The important aspect of the present study is the analysis of the results of the treatment of patients under local anesthesia. This approach provides undeniable advantages because it gives the possibility of early diagnostics of serious complications, especially neurological deficits. Spinal cord ischemia is still one of the most severe complications of endovascular reconstruction of thoracic aorta, and the performing operations under local anesthesia is another step towards early diagnostics of spinal cord ischemia that allows to reduce its symptoms in case of the occurrence [9].
The limitations of the study. The limitation is retrospective analysis and inability to perform propensity score matching because of a small group of patients.
Conclusion
Routine use of percutaneous puncture method and local anesthesia in stable patients while performing endoprosthetic repair of thoracic aorta, showed high efficiency and safety. The combination of local anesthesia and percutaneous puncture access in concerned with less number of complications that are typical of traditional surgical access under general endotracheal anesthesia. As a result, the duration of hospitalization and rehabilitation is reduced, and, together with other factors, all this is more favorable for the patients. Without general anesthesia, it is possible to conduct a constant neuromonitoring. This contributes to early detection of neurological complications. We believe that the most reliable closure of the arterial wall defect is carried out using a combination of suturing devices. This allows to safely apply the large caliber delivery devices up to 25F. The risks of cutaneous sensitivity disorders, lymphorrhea and infection are minimized. The duration of the operation is significantly reduced. In most cases, there is no need to monitor the patients in early postoperative period in the intensive care unit. And there is also the possibility of early mobilization of the patient. All these factors can significantly reduce the time of hospitalization and economic costs.
Relationships and Activities: none.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Gaponov D.P., Khafizov T.N., Kochkina K.V., Chernov I.I., Enginoev S.T., Shaposhnikova E.I. Comparison of open femoral exposure and percutaneous access in endovascular reconstruction of the thoracic aorta: a two-center retrospective study. Russian Journal of Cardiology. 2022;27(3S):5135. https://doi.org/10.15829/1560-4071-2022-5135
Copy