Cardiovascular system status of long-livers in Moscow: the prevalence of cardiovascular diseases and their risk factors
Over the past century, there has been an increase in life expectancy: from 1950 to 2017, the mean life expectancy increased from 48,1 to 70,5 years for men and from 52,9 to 75,6 years for women [1]. At the same time, the number of long-livers and centenarians is increasing: people who have reached the age of 85 and 100 years, respectively. According to calculations of the United Nations (UN) by 2100, the number of centenarians worldwide will reach 25 million people [2].
In Russia, the same trends are observed: the annual growth of long-livers since 2014 is 600-900 people per year, and by 2019, 20582 centenarians (5895 men and 14687 women) live in the country [3].
Cardiovascular diseases (CVDs) have been the leading cause of death for people 65 years of age and older in Russia and in the world for at least the last 20 years. Despite the increase in the number of centenarians, to date, the state of cardiovascular system and the main cardiovascular risk factors (RF) have been little studied in this age group.
The aim was to assess the state of cardiovascular system, the prevalence of CVDs and related main risk factors (RFs) among centenarians.
Material and methods
The study protocol was approved by the independent ethics committee of the Pirogov Russian National Research Medical University, Russian Clinical and Research Center of Gerontology (meeting № 02/15 dated February 12, 2015). This study is registered with ClinicalTrials.gov № NCT02876809. The study recruitment was initiated in 2015: 82 residents of Moscow aged 95 and older were included, who personally (if impossible, with the help of relatives or guardians) agreed to undergo the examination. Fifty-one participants underwent echocardiography, while 64 — laboratory examination, including biochemical analysis and complete blood count.
The inclusion criterion was age 95 and older. There were no exclusion criteria, with the exception of refusal to participate in the study.
Patients were seen at home in the presence of a social worker and/or the patient’s relatives.
History was collected by patient’s and/or his relatives’ account. To identify chronic diseases and analyze the therapy taken, when possible, data from available medical records were used.
We collected data on weight and height and then calculated the body mass index (BMI). BMI <18,5 kg/m2 was considered as underweight, from 18,5 to 24,9 kg/m2 — normal body weight, from 25 to 29,9 kg/m2 — overweight, and 30 or more kg/m2 — obesity [4].
The study of the lipid profile and glycated hemoglobin levels was carried out using an AU 680 (Beckman Coulter) clinical chemistry system.
There were following reference values for lipid profile parameters: <5,0 mmol/L for total cholesterol (TC), 3,5 mmol/L for low density lipoproteins (LDL) and <1,7 mmol/L for triglycerides (TG). For men, the level of high-density lipoproteins (HDL) was considered low at <1,2 mmol/L, and for women — 1,0 mmol/L [5].
Ultrasound of the heart and main arteries was performed using a Samsung Medison U6 portable ultrasound machine. Cardiac structure and function was assessed using the normal ranges from 2012 Russian Society of Cardiology guidelines [6]. Vascular stiffness was determined using SphygmaCor technology (AtCor, Sydney, Australia).
Statistical data processing was performed using the SPSS 23.0 program (SPSS Inc., USA). Due to the small number of observations, the analysis of quantitative traits’ distribution was not carried out. Quantitative variables are presented as Me (25%; 75%), where Me is the median, 25% — 25th percentile, 75% — 75th percentile, since the data is not normally distributed.
Results
The mean age was 98,3 (95-105) years, of which 72 (87,8%) were women. At the same time, the age of 66 participants in the study was from 95 to 99 years old and 16 was 100 years old or more.
Risk factors. The majority of long-livers never smoked (n=73; 89%), while 8 (9,8%) participants were former smokers, and one (1,2%) continued to smoke (up to 5 cigarettes a day). The median duration of smoking among smokers was 5 years (range 1 to 65 years).
Alcohol consumption was not widespread among long-livers: 78 people (95,1%) drank alcohol-containing products 2-3 times a year (up to 2 glasses per meal), and 4 (4,9%) drank alcohol regularly.
For the most part, centenarians led a sedentary lifestyle (56 (68,3%)). The minority regularly went for walks (18 (22%)) or did morning exercises (7 (8,5%)). Of these 25 people (30,5%), 16 (19,5%) spent up to 30 minutes a day on sports, 4 (4,9%) — up to 1 hour, and the remaining 5 (6,1%) — more than an hour.
Obesity and overweight were in 6 (7,3%) and 28 (34,1%) study participants, respectively.
Thus, the classic RFs for CVD were the exception rather than the rule among participants (Figure 1).
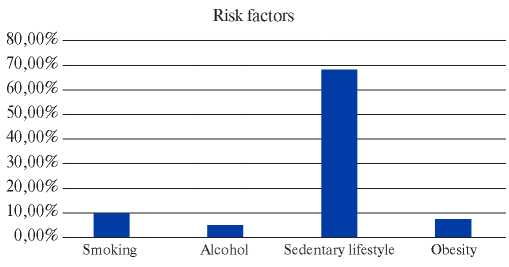
Figure 1. Prevalence of conventional RFs (n=82).
CVD. The most common diseases among the study participants were hypertension (64 (78%)), coronary artery disease (CAD) (42 (51,2%)) and heart failure (HF) (26 (31,7%)). Acute myocardial infarction (MI) or stroke were significantly less common — in 16 (19,5%) and 17 (20,7%) participants. Occlusive peripheral arterial disease and atrial fibrillation were extremely rare: (3 (3,7%)) and (7 (8,5%)), respectively (Figure 2).
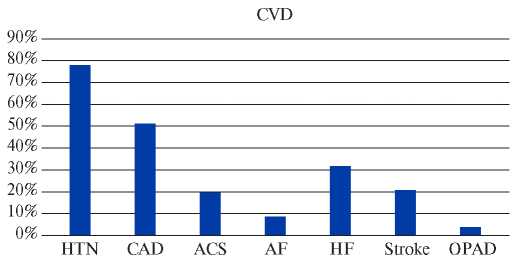
Figure 2. CVD prevalence among participants (n=82).
Abbreviations: HTN — hypertension, CAD — coronary artery disease, ACS — acute coronary syndrome, AF — atrial fibrillation, HF — heart failure, OPAD — occlusive peripheral arterial disease.
Therapy. One of the most widespread drugs among long-livers was acetylsalicylic acid as primary (20 (24,4%) and secondary prevention of CVD (14 (17,1%)).
The most frequently prescribed antihypertensive therapy were angiotensin-converting enzyme inhibitors (25 (30,5%)) and beta-blockers (22 (26,8%)). Significantly less frequently, patients took angiotensin II receptor blockers (13 (15,9%)) and calcium channel blockers (16 (19,5%)).
Slightly less than a quarter (17 (20,7%)) received diuretic therapy (thiazide and loop diuretics). Five (5,6%) subjects took long-acting nitrates. None of the patients with atrial fibrillation took anticoagulants (Table 1).
Table 1
Medicines taken by study participants (n=82)
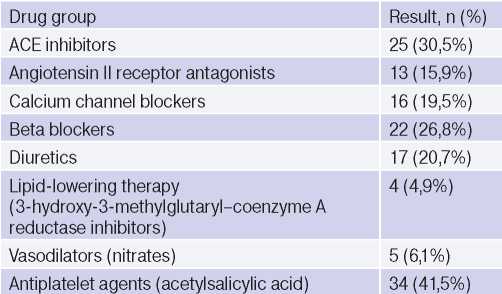
Abbreviation: ACE — angiotensin converting enzyme.
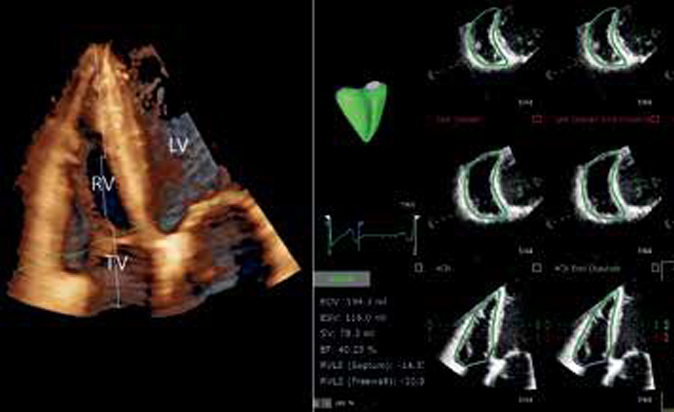
Cardiac ultrasound. Echocardiography was performed in 51 study participants. There were following echocardiographic findings: left atrium (LA) dilation (74,5%), interventricular septum thickening >1,1 cm (100%), increased pulmonary artery pressure >30 mm Hg (48%) and left ventricular (LV) diastolic dysfunction (32%). Systolic dysfunction was observed in 2 (3,9%) subjects (Tables 2, 3).
Table 2
Results of echocardiography (n=51)
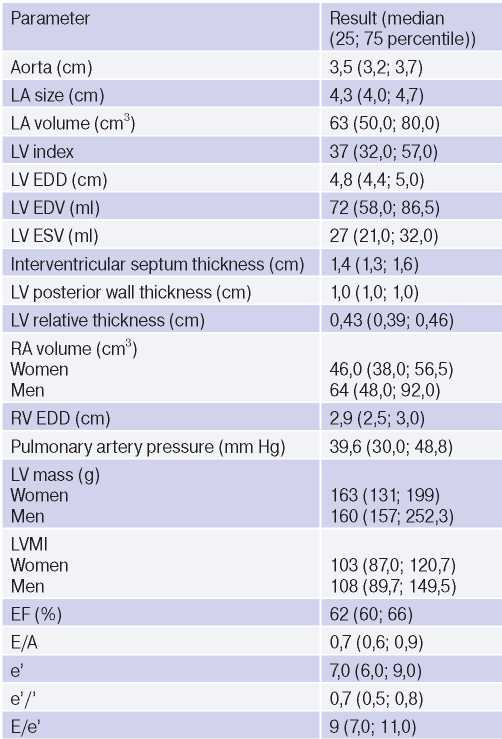
Abbreviations: LVMI — left ventricular mass index, EDV — end diastolic volume, EDD — end diastolic dimension, ESV — end systolic volume, LV — left ventricle, LA — left atrium, RA — right atrium, RV — right ventricle, EF — ejection fraction.
Table 3
Prevalence of echocardiographic abnormalities among centenarians (n=51)
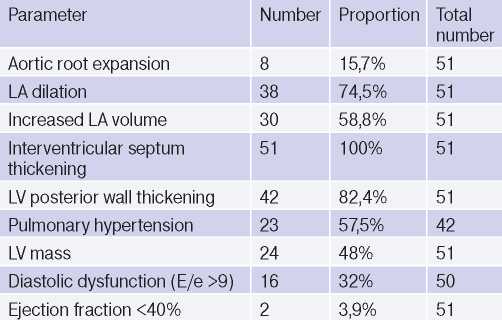
Abbreviations: LV — left ventricle, LA — left atrium.
Ultrasound of carotid and femoral arteries. All long-livers had atherosclerotic plaques in the common carotid (CCA) and femoral arteries (mean, 5). However, hemodynamically significant stenoses (70% or more) were extremely rare: 3 and none in the CCA and femoral artery systems, respectively. The median intima-media thickness in the CCA system was approximately 1 mm, while in the femoral one — 1,5 mm (Table 4).
Table 4
Results of duplex ultrasound of main arteries (n=65)
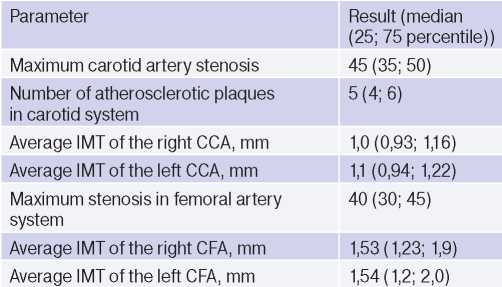
Abbreviations: CFA — common femoral artery, CCA — common carotid artery, IMT — intima-media thickness.
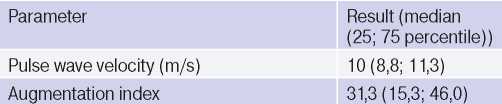
Vascular stiffness. The vascular stiffness was determined in 67 centenarians, of which the median pulse wave velocity was 10 m/s, and the augmentation index was 31,3 (Table 5).
Table 5
Results of vascular stiffness examination (n=64)
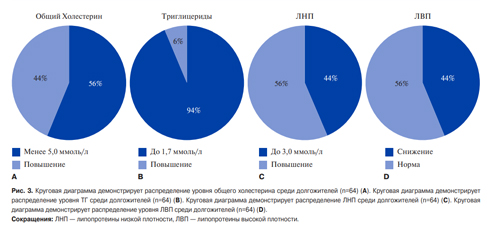
Lipid profile. The lipid profile was analyzed in 65 study participants. According to formal criteria, dyslipidemia was found in 55%. Three patients continued to take statins (atorvastatin at a dose of 10-20 mg a day). An increase in TC >5,0 mmol/L was in 55% (3,0-7,5 mmol/L), TG >1,7 mmol/L — in 5,3% (0,6- 1,8 mmol/L), LDL >3,0 mmol/L — in 44% (1,7-5,5 mmol/L), and a decrease in HDL <1,0 mmol/L — in 43% (0,7-2,8 mmol/L) (Figure 3).
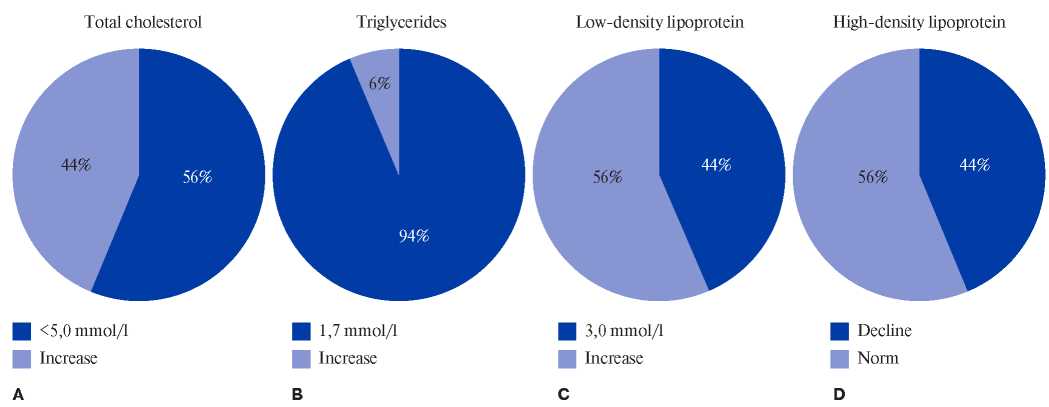
Figure 3. The pie chart shows the distribution of TC levels among centenarians (n=64) (A). The pie chart shows the distribution of TG levels among centenarians (n=64) (B). The pie chart shows the distribution of LDL levels among centenarians (n=64) (C). The pie chart shows the distribution of HDL levels among centenarians (n=64) (D).
Abbreviations: LDL — low-density lipoprotein, HDL — high-density lipoprotein.
Discussion
A healthy lifestyle, regular physical activity, healthy balanced diet, freedom from nicotine and alcohol products reduces the risk of CVD and cancer and, as a result, increases the duration of an active life in general.
Smoking (1,2%) and alcohol consumption (4,9%) are not very common among long-livers in Moscow. International data on this issue vary: in the Italian GEHA register, 3,2% of participants smoked [7]; in the Chinese Dijiangyan Study — 43% [8]. The same variability can be traced with regard to alcohol consumption: just over 50% of centenarians in Italy consumed 1 glass of wine per day throughout their lives, among Chinese centenarians — 27% (however, the volume and frequency of alcohol consumption is not indicated). It was typical for Moscow centenarians to drink alcoholic beverages on holidays and in a little amount (Social drinking).
Most of the patients led a sedentary lifestyle (68,3%) at the time of inclusion in the study, and 7,8% did exercise and 22% went for a walk regularly, but the majority of centenarians during the survey reported that they had an active lifestyle in youth and maturity. These results are inferior to the Italian GEHA data, where 37% did daily walking [7], and the Chinese, where up to 40% did daily exercise [8].
Overweight among young and middle-aged people is a well-known RF for CVD. Among older age people, BMI ceases to be such an unambiguous unfavorable factor. Recent studies have shown that among older patients, a low and normal BMI (<23) is associated with higher mortality than those who had it in the range from 23 to 32 (which corresponds to overweight and even partially class 1 obesity) [9]. Among the study participants, underweight and obesity were quite rare — 13,4% and 7,3%, respectively. There was no significant difference in BMI between survivors and deaths.
Severe dyslipidemia was not widespread among centenarians of Moscow and generally corresponded to the international data from Italy (TC, 5,2±1,2 mmol/L; LDL, 3,1±0,9 mmol /L) and China (TC, 4,2±0,8 mmol/L; LDL, 2,3±0,7 mmol/L) [7, 8].
A feature of centenarians is the late development of aging-associated diseases, including CVD [10]. Among centenary veterans of the United States, the prevalence of hypertension was 45%, CAD — 20%, MI — 15% and HF — 32%) [10]. The prevalence of hypertension and CAD was higher among Moscow centenarians, while the incidence of MI and HF was comparable.
In the literature there is little data on instrumental diagnostic tests of centenarians. Doppler ultrasound of the pulse wave of Okinawa long-livers demonstrated that, in general, the pulse wave velocity was <10 m/s, which is typical for younger patients [11] and correlates with the results of the Moscow study.
We have demonstrated the following patterns: LA dilation, increased LV mass, interventricular septal thickening, widespread pulmonary hypertension and diastolic dysfunction among the study participants.
All the data obtained correspond to the structural and functional cardiac abnormalities that occur with age. Thus, the Framingham study demonstrated that the prevalence of LA dilation increases with age and correlates with RFs for CVD [12]. Another agingassociated change is LV diastolic dysfunction; its incidence doubles every decade starting at age 65 in men, and triples in women. In 2008, discrete upper septal thickening (DUST) was described for the first time [13]. The prevalence of this phenomenon is directly proportional to age and, according to the Framingham study, reaches 18% among people over 85 years old. The question remains about the good quality of these changes and their impact on the human condition. There is evidence that hypertrophy of the interatrial septal basal part does not affect the normal rest function of a person, but can limit his physical activity, causing limitation of blood flow through the aortic valve [13]. It has also been shown that the prevalence of diastolic dysfunction in different age groups varies and can reach 50% among healthy volunteers aged 65 and over [14].
Despite the rather large number of atherosclerotic plaques in the common carotid and femoral arteries, the number of hemodynamically significant plaques was minimal. An intima-media thickening up to 1,0- 1,1 mm was found, which corresponds to the estimated age norm for centenarians [15].
A study limitation is the design, which does not allow for clarification of causal relationships.
Conclusion
Over the past century, there has been a steady trend towards an increase in life expectancy. Longlivers in Moscow are characterized by a low prevalence of conventional RFs for CVD (with the exception of hypertension) and a fairly high prevalence of structural and functional cardiac and vascular abnormalities.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Eruslanova K.A., Luzina A.V., Onuchina Yu.S., Ostapenko V.S., Sharashkina N.V., Alimova E.R., Akasheva D.U., Bazaeva E.V., Ershova A.I., Drapkina O.M., Kotovskaya Yu.V., Runikhina N.K., Tkacheva O.N. Cardiovascular system status of long-livers in Moscow: the prevalence of cardiovascular diseases and their risk factors. Russian Journal of Cardiology. 2021;26(1S):4028. (In Russ.) https://doi.org/10.15829/1560-4071-2021-4028
Copy