Ренальная денервация в лечении вторичной артериальной гипертензии. Клинический случай

Аннотация
Введение. Вазоренальная артериальная гипертензия (АГ) является одной из наиболее тяжелых, в плане выбора тактики лечения, форм АГ. Исследования последних лет не позволили получить однозначный ответ о том, какой метод лечения — медикаментозный или хирургический — является выбором для данных пациентов.
Краткое описание. Представленный клинический случай показывает наблюдение за пациенткой с длительным анамнезом неконтролируемой АГ, при обследовании которой выявлено двухстороннее стенозирование почечных артерий. Учитывая дискутабельность клинической эффективности реваскуляризации стеноза почечных артерий, пациентке проведена ренальная денервация дистальных сегментов с использованием многоэлектродных катетеров. Показано снижение уровня артериального давления. Наблюдение за пациенткой продемонстрировало сохранение антигипертензивного эффекта процедуры, а также ее безопасность при скомпрометированной почкой.
Дискуссия. Данный клинический случай демонстрирует наличие третьего пути в лечении пациентов со стенозирующим атеросклерозом почечных артерий с формированием резистентной АГ — симпатической денервации почечных артерий. Применение данного метода требует проведения отдельного контролируемого исследования с включением лиц с почечной дисфункцией, в т.ч. реноваскулярного генеза.
Introduction
Despite the prior progress, arterial hypertension (AH) remains one of the main modifiable risk factors for the development of adverse cardiovascular complications, accounting for 19,2% (16,9-21,3%) of all deaths in the world [1]. One of the reasons for this is the low control of blood pressure (BP) in the population, so according to epidemiological studies in the Russian Federation, the proportion of people who have reached a BP level of less than 140/90 mm Hg is 24,9% (34,1% of women and 16,5% of men) [2]. A possible reason for this is symptomatic hypertension; vasorenal hypertension is common, the leading mechanism of which, atherosclerosis of the renal arteries, is detected in 6,8% of patients older than 65 years [3]. According to published data, there is no consensus on the efficacy and safety of revascularization in renal artery stenosis. Studies have not demonstrated the benefits of renal artery stenting in borderline stenosis compared with medical therapy, and significant complications after the procedure were noted in the STAR study [4][5].
Patients with vasorenal AH still remain one of the most difficult cohorts, despite the positive trends in the diagnosis and treatment of the pathology. Clinical practice often suspects renal artery stenosis based on certain symptoms, including the development of severe AH in people older than 55 years, uncontrolled, often resistant AH, decreased kidney size (often on one side), and recurrent pulmonary edema while BP is rising quickly [6]. However, the diagnosis is based primarily on the use of duplex scanning of renal arteries, computer tomography-angiography of renal arteries, and, in rare cases, magnetic resonance imaging with gadolinium. Furthermore, the choice of treatment strategies for patients with renovascular AH presents significant challenges. Today, researchers frequently identify two approaches: drug treatment and revascularization. Defining indications for renal artery revascularization presents some challenges. According to the consensus documents, renal artery stenting may be helpful when the stenosis level is more than 70%. However, studies have not shown any benefits when the stenosis level is less than 50% in terms of lowering BP or improving kidney function. Simultaneously, a zone of 50-70% appears to exist where the presence of positive effects of renal artery revascularization remains uncertain [4].
To date, there is limited data demonstrating the possibility of using sympathetic denervation of renal artery (RD) in renovascular hypertension. This clinical case presents the observation of a patient with renovascular disease after renal denervation.
Case Study
Patient H, 60 years old, was admitted to the cardiology department of the Emergency Hospital with acute left ventricular failure and increase in BP to 240/130 mm Hg. From the medical history, it is known that BP has been elevated to 210/120 mm Hg for 10 years. The patient was hospitalized twice in the past year for complicated hypertensive crisis, at the time of hospitalization in 2021, according to duplex scanning of the renal arteries (at the source of the renal arteries, Vps 70 cm/s on the right and 72 cm/s on the left, resistance index (RI) 0,76 on both sides) revealed bilateral stenosis of the renal arteries. Since the same time, correction of therapy — withdrawal of drugs blocking the renin-angiotensin-aldosterone system was carried out. Against the background of combined therapy (amlodipine 10 mg/day, nebivololol 5 mg/day, indapamide 2,5 mg/day and moxonidine 0,4 mg/day) the hemodynamics were adjusted to 160/100 mm Hg. The patient is also known to suffer from type 2 diabetes for 5 years, for which he takes metformin 1000 mg/day. After stabilization during this hospitalization, his BP remained at the level of 170-180/110-120 mm Hg in spite of the combined therapy.
The anamnesis also noted the presence of a nodular goiter with euthyroidism (the patient lives near the former Semipalatinsk nuclear test site, which is known for thyroid diseases with nodular formation).
On admission, the patient’s condition was severe. Consciousness is clear. There was marked dyspnea. The skin was of normal color and moist. We heard vesicular breathing above the lungs, with moist, fine, bubbly rales in all fields and a respiratory rate of 28/min. The first point muffled heart tones, and a 2-tone accent was audible above the aorta. The BP measured 240/130 mm Hg, and the heart rate was 88 beats per minute. The pulse was regular and tense. The abdominal cavity showed no abnormalities. We detected a small edema in the lower legs. Diuresis was independent.
On admission, laboratory data revealed chronic kidney disease with a creatinine level of 122 μmol/l and glomerular filtration rate according to CKD-EPI of 44 ml/min/1,73 m2. According to urine analysis data, an albumin to creatinine ratio of 50 mg/g was detected (reference range: less than 30 mg/g).
Electrocardiography recorded sinus rhythm with heart rate of 90 per min, signs of left ventricular (LV) hypertrophy. Echocardiography demonstrated preserved LV ejection fraction (65% according to Teicholtz), as well as LV myocardial mass index was 118 g/m2. Ambulatory Blood Pressure Monitoring revealed severe systolic-diastolic AH during the day with a mean BP of 177/97 mm Hg. Ultrasound examination of renal arteries revealed altered blood flow at the nutrient renal level, with a resistance index value of more than 0,7 on 2 sides, a systolic pressure gradient of 15-17 mm Hg.
To assess renal hemodynamics, the patient underwent nephroangiography: right renal artery diameter was 5,3 mm with proximal segment stenosis up to 60-65%; left renal artery diameter was 4,9 mm and proximal third stenosis 60%.
Final diagnosis: Grade III AH, very high risk of cardiovascular complications. Uncontrolled AH. Atherosclerosis of the renal arteries causes ischemic kidney disease. The patient suffers from chronic heart failure of functional class III (NYHA) and maintains a preserved LV ejection fraction. Diabetes mellitus type 2 compensation. AH, diabetic nephropathy, and ischemic kidney disease cause chronic kidney disease of mixed genesis, which is at stage C3b.
Given the detected borderline bilateral stenosis of the renal arteries, lack of convincing data demonstrating the benefits of renal artery revascularization, it was decided to perform RD (Figure 1).
Renal denervation procedure was performed using Siemens Artiz Zee angiographic unit (Germany). The premedication was performed 30-40 minutes before the intervention. The procedure was performed by transfemoral access on the right side. After local anesthesia with 2% Lidocaine solution, we performed arterial puncture according to the Seldinger method with installation of a 6 Fr introducer. Visualization of the renal arteries was performed in the anteroposterior view by means of abdominal aortography using a PigTail 5 Fr diagnostic catheter. The SDRA procedure was performed using a 2nd generation catheter — Symplicity Spyral Renal Denervation System Catheter (Medtronic Inc., Minneapolis, Minnesota, USA). 18 ablations in each renal artery using distal RD technique were performed (ablation in the terminal part of the renal artery trunk and segmental branches) (Figure 2).
There were no complications in the early post-operative period. On the 7th day BP was 155/89 mm Hg. There was a slight increase in creatinine up to 125 μmol/l with a glomerular filtration rate of 43 ml/min/1,73 m2.
The patient continued therapy (metoprolol 100 mg twice daily, amlodipine 10 mg/day, indapamide 2,5 mg/
day, and sacubitril/valsartan 200 mg/day) after RD. Correction of antidiabetic therapy was also performed — dapagliflozin 10 mg/day was recommended.
A nephrologist also repeatedly consulted with the patient. Additional conservative therapy was agreed upon. A multidisciplinary team consisting of a cardiologist, a nephrologist, and an endocrinologist will monitor the patient every month for three months following the intervention and every three months after that.
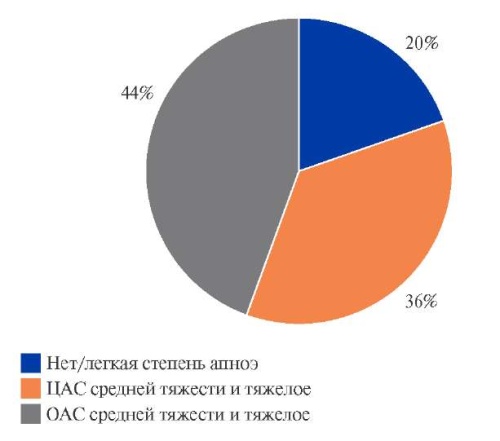
The follow-up after 6 months showed preservation of the antihypertensive effect of RD, although the BP level remained above the target level, the mean BP level was 141/88 mm Hg (Figure 3).
An important aspect is slowing the progression of chronic kidney disease, the creatinine level decreased to 114 mmol/l, glomerular filtration rate was 48 ml/min/1,73 m2. Echocardiography revealed regression of LV hypertrophy, LV myocardial mass index was 107 g/m2.


Figure 1. Right and left renal artery. The arrow indicates the location of the stenosis.


Figure 2. Positioning of the spiral catheter in the renal artery on the right and left side.

Figure 3. Variations of BP levels before RD, as well as after 7 days and 6 months.
Abbreviation: RD — renal denervation.
Discussion
After a period of disappointment, there is currently an increased interest in the RD procedure. Data available up to now have shown the safety and efficacy of radiofrequency and ultrasound catheter denervation use in the treatment of resistant hypertension [7-9]. However, the most controversial and limiting issue is the selection of patients for this procedure. According to published papers [9][10], the main indications for RD are resistant essential AH. However, there are data on the possibility of performing a catheter procedure in patients with secondary hypertension, provided that it is impossible or ineffective to use methods for correcting the prior pathology [10][11].
Basic research of G. Grassi [12] confirmed that chronic sympathetic overdrive is one of the cornerstone components of the development of hypertension, as well as the progression of target organ damage. Hyperactivity of the sympathetic nervous system is directly related to the progression of renal failure [13]. The results of experimental studies have confirmed that the destruction of the afferent renal nerves leads not only to a decrease in BP, but also to a slowdown in the progression of renal dysfunction in ischemic and non-ischemic kidneys [14], which theoretically determines the possibility of using RD in renovascular disease. According to ESH guidelines, radiofrequency denervation of renal arteries now has enough evidence to be used more often in real clinical settings. However, experts only recommend it for resistant AH and say that symptomatic forms should not be used [15]. The expert consensus on the use of renal denervation in the Russian Federation also prefers only refractory (including resistant) essential hypertension [10].
There is limited data on the use of renal denervation in renovascular hypertension. So, in the paper of Ziegler AK, et al. an example of the use of RD in a 69-year-old patient with uncontrolled hypertension despite previous stenting of the proximal segments of the renal arteries was demonstrated [16]. In this clinical case, given the «gray zone» of the lesion (arterial stenosis about 60%), according to the consensus of American Heart Association [3], there is insufficient evidence for renal artery stenting. Thus, it was decided to carry out at this stage renal denervation in the distal segments of the renal arteries using a multi-electrode catheter. In this case, the distal localization of radiofrequency exposure has advantages, since it is in the distal segment that a closer contact of the true sympathetic plexuses with the artery wall is detected [17]. Of undoubted interest is the preservation of the clinical effect during the observation period of our patient for 6 months.
In addition, in a published series of cases (10 patients), also in patients after renal artery recanalization, renal denervation contributed to a decrease in BP levels by 7,6/3,1 and 11,3/5,1 mm Hg after 6 and 12 months respectively [18]. In our case, a decrease in BP to mm Hg was also achieved up to 141/88 mm Hg.
Conclusion
Sympathetic denervation of the renal arteries may be one of the treatment strategies for patients with uncontrolled AH and renal artery stenosis. In this case, in addition to immediate reduction of BP level, some nephroprotective effect of the procedure can be expected. However, lack of clinical trials limits the use of this method, thus certainly requires participation of patients with renovascular hypertension in further randomized clinical trials.
Informed consent to the use of medical data for scientific purposes has been obtained.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Ключевые слова
Для цитирования
Орехов А.Ю., Каражанова Л.К., Чиныбаева А.А., Жаксебергенова А.Б. Ренальная денервация в лечении вторичной артериальной гипертензии. Клинический случай. Российский кардиологический журнал. 2024;29(3S):5784. https://doi.org/10.15829/1560-4071-2024-5784. EDN: FVKYNO
Скопировать