Short-term outcomes of Ozaki procedure: a multicenter study
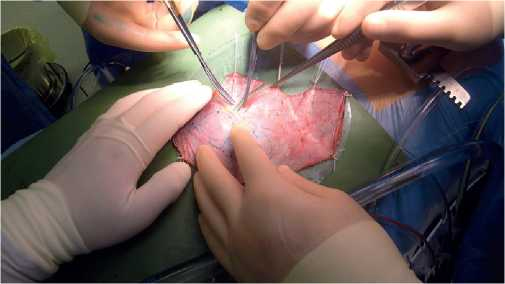
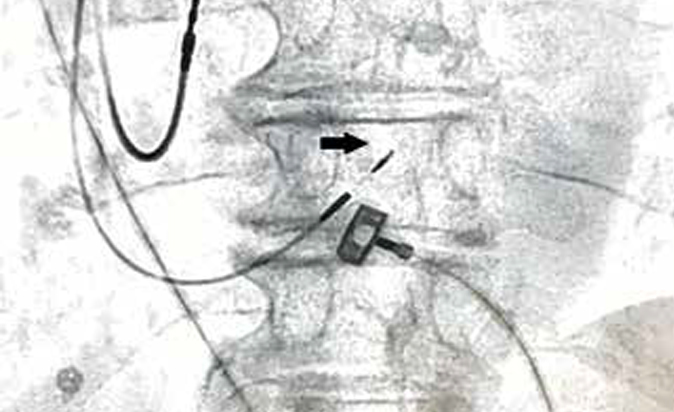
Aortic valve (AV) replacement is the gold standard in the treatment of AV disease. There are cases that lead to a prosthesis-patient mismatch after AV replacement with both mechanical and biological prosthe- ses, especially in patients with a small aortic annulus (AA) [1]. In 2011, Ozaki Sh, et al. [2] reported on their method of AV neo-cuspitization (AVNeo), ie, AV replacement with glutaraldehyde-treated autologous pericardium (Figure 1), using special templates (Figure 2). Considering that this technique is new and not many centers perform this operation, in 2019 we created the Russian AVNeo register to assess short- and long-term outcomess. Our first short-term results were published with 170 patients after AVNeo [3]; a little later, the results of surgical treatment of patients with small AA with good short-outcomes were reported [4]. In this study, we want to analyze the short-term outcomes of the register, to find out if AVNeo is an acceptable and reproducible technique.
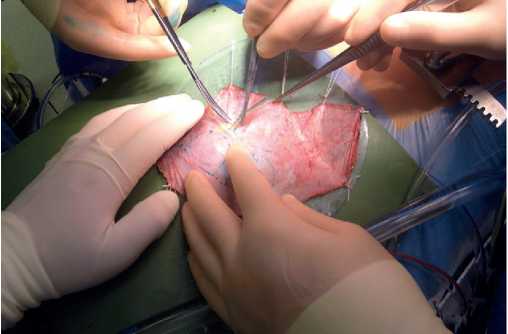
Figure 1. One of the Ozaki procedure stages: excision of the glutaraldehyde-treated pericardium for the AV replacement.
Material and methods
Study design. We performed the retro-prospective multicenter study of patients with AV disease selected for the Ozaki procedure. The study was approved by the local ethics committee of each participating institution.
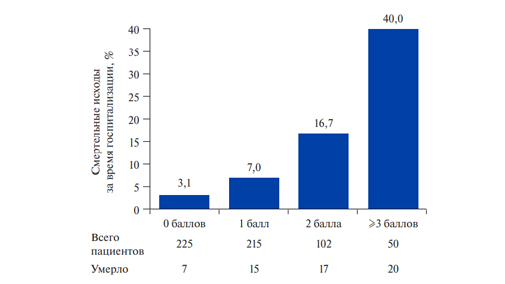
Echocardiographic data. All patients underwent AV echocardiography before and after surgery. The maximum and mean AV gradient, the effective orifice area (EOA) (Figure 3), aortic regurgitation (AR) degree, including structural, Doppler, quantitative and qualitative parameters recommended by the American Society of Echocardiography [4], was assessed. For the classification of prosthesis-patient mismatch, guidelines for visualization of artificial heart valves were used [5].
End points. The primary endpoints were in-hospital mortality and hemodynamic echocardiographic after AVNeo. Secondary endpoints were postoperative complications: arrhythmias requiring permanent pacing; stroke; infectious complications; acute renal failure (requiring hemodialysis).
A total of 724 patients were included in the registry, who were operated on from 2015 to 2019 (Figure 4). Among the patients, as shown in Table 1, there were 395 (54,5%) men and 329 (45,5%) women. The median age of the patients was 63 (5767) years. The minimum age was 10 years and the maximum age was 83 years (Figure 5). Most of the patients were over 60 years old.
Table 1
Initial characteristics of the patients and risk factors
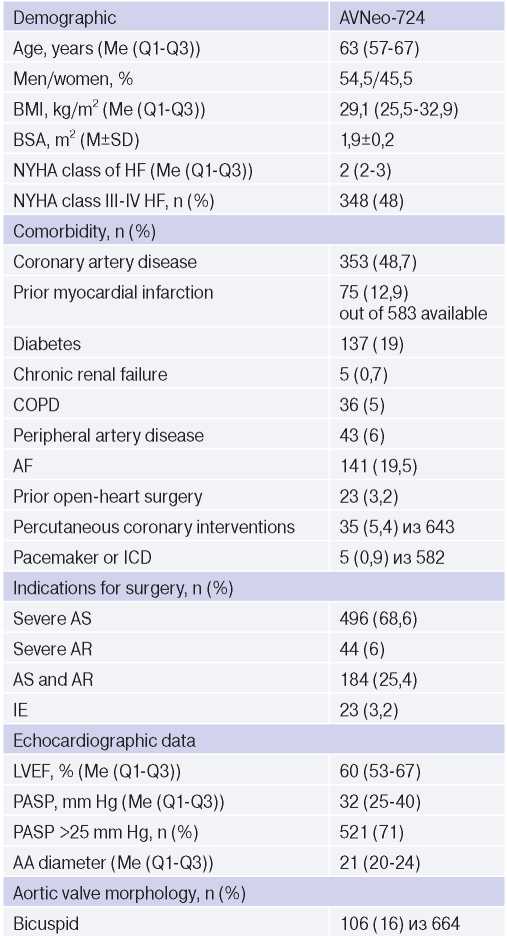
Abbreviations: ICD — implantable cardioverter defibrillator, AR — aortic regurgitation, AS — aortic stenosis, CAD — coronary artery disease, BMI — body mass index, IE — infective endocarditis, BSA — body surface area, PASP — pulmonary artery systolic pressure, LVEF — left ventricular ejection fraction, AF — atrial fibrillation, COPD — chronic obstructive pulmonary disease, CRF — chronic renal failure, HF — heart failure, NYHA — New York Heart Association.
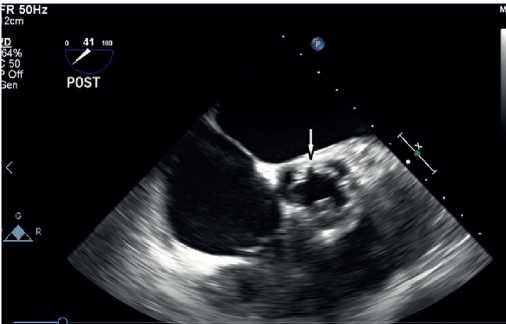
Figure 3. Aortic valve effective orifice area after Ozaki procedure
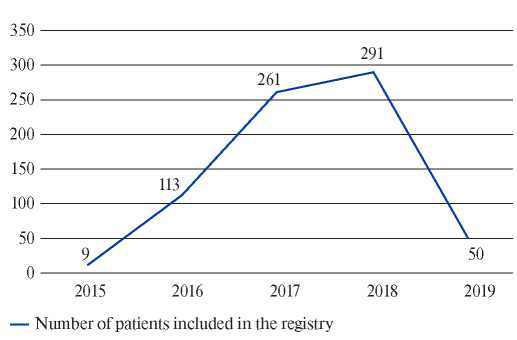
Figure 4. Number of patients included in the registry
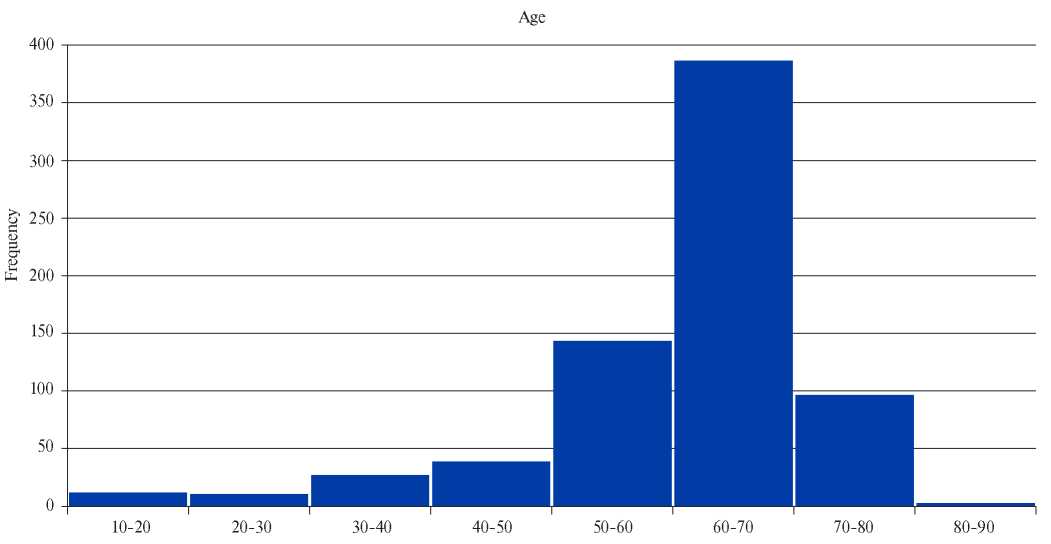
Figure 5. Age of patients included in the registry
The most common causes of AV dysfunction were aortic stenosis — 496 (68,6%) patients, AR — 44 (6%), aortic stenosis and AR — 184 (25,4%) patients. Infective endocarditis as a cause of AV disease was diagnosed in 23 (3.2%) patients. Manifested class III-IV heart failure occurred in 348 (48%) patients. Every fifth patient has a history of atrial fibrillation. The number of valves was estimated in 664 patients, and bicuspid AV was diagnosed in 106 (16%) patients. Preoperative echocardiography revealed the median AA of 21 (20-24) mm, systolic pulmonary artery pressure (SPAP) of 32 (25-40) mm Hg, SPAP >25 mm Hg in 521 (72%) patients, left ventricular ejection fraction of 60 (53-67)%. Patient baseline characteristics and risk factors are presented in Table 1.
Statistical analysis. Statistical processing was performed using the IBM SPSS Statistics 26 software package (Chicago, IL, USA). All quantitative variables were analyzed for the distribution type using the Kolmogorov-Smirnov test. Central tendencies and scattering of quantitative traits, having a normal distribution, were described as the mean and standard deviation (M±SD). In the case of a nonnormal distribution, this was presented as median (interquartile range of the 25th and 75th percentiles) and Me (Q1-Q3). In most samples, a nonparametric distribution was revealed.
Results
Peri- and postoperative data. In total, 314 (43,4%) patients underwent an isolated AVNeo, and the remaining 410 (56,6%) patients underwent combined interventions. Access to the heart was performed through a median sternotomy in 687 (95%) patients, and in 37 (5%) patients through a mininotomy. The median extracorporeal circulation time was 130 (110-130) min, and the time of myocardial ischemia was 104 (86-122) min (Table 2). Inhospital mortality rate was 1,6% (Table 3). Thirteen (1,8%) patients received a pacemaker. Acute renal failure was diagnosed in 4 (0,5%) patients, stroke — in 3 (0,4%), sternal infection — in 10 (1,4%) (Table 3).
Table 2
Intraoperative parameters

Abbreviations: AV — aortic valve, CABG — coronary artery bypass grafting.
Table 3
Postoperative results

Abbreviations: AV — aortic valve, IE — infective endocarditis, ARF — acute renal failure.
Postoperative echocardiography. The maximum and mean AV pressure gradients after surgery were 10,9 (7,4-14,8) mm Hg and 5,3 (3,5-7,3) mm Hg, respectively. AV EOA and EOA index after surgery were 3 (2,5-3,9) cm2 and 1,6 (1,32) cm2/m2, respectively. One (0,1%) patient had a moderate patient-prosthesis mismatch and one (0,1%) had a pronounced one. After the AVNeo, 11 patients (1,5%) had moderate AR and 1 (0,1%) had severe AR. A patient with severe AR underwent AV replacement before discharge from the hospital (Table 4).
Table 4
Postoperative echocardiographic parameters

Abbreviations: AV — aortic valve, AR — aortic regurgitation, EOA — effective orifice area, LVEF — left ventricular ejection fraction.
Discussion
Autologous pericardium has been regularly used since the early cardiac surgery. In 1963, Bjoerk VO and Hultquist G [6] performed AV replacement by creating valves from the autologous pericardium. In 2011, Ozaki Sh, et al. [2] reported on their method of AV neo-cuspitization (AVNeo) with glu- taraldehyde-treated autologous pericardium, using special templates treated. There is also a website (www.avneo.net), which contains useful information related to AVNeo. AVNeo can be considered an attractive option due to its low cost, universal indications without any restrictions related to the AA size and need for anticoagulation, as well as potentially excellent hemodynamic parameters after surgery. The most important results of our study were low mortality rate (1,6%) (Table 3). According to Fallon JM, et al. [8], after AV replacement with various prostheses, the frequency of moderate and pronounced patient-prosthesis mismatch occurs in 54% and 11% of cases, respectively. The same authors [7] have shown that any “patient- prosthesis” mismatch significantly reduces longterm survival and increases the rehospitalization rate for both heart failure and reoperations. According to our data, only in 0,1% of cases there was a moderate and pronounced patient-prosthesis mismatch (Table 4). The multicenter study [4] from our registry has been published: AVNeo (Ozaki procedure) in patients with AA <21 mm. The mean AA diameter was 19,8±1,1 mm. The maximum and mean pressure gradients after surgery were 11,8±5,9 mm Hg and 7,3±3,5 mm Hg, respectively. EOA and EOA index averaged 2,5±0,4 cm2 and 1,3±0,3 cm2/m2 after surgery, respectively. According to our registry, the AA diameter before surgery was measured in 458 patients, of which 256 (56%) patients had AA <21 mm. Rosseikin EV, et al. [8] compared mininotomy and complete median sternotomy during Ozaki procedure. The duration of the operation and cardiopulmonary bypass was longer in the mininotomy group, but the groups did not differ in myocardial ischemic time. There were also no significant differences in other endpoints. In our study, mininotomy was performed in 5% of cases. Several studies [9, 10] have reported excellent results with Ozaki procedure in children. Currently, our registry includes 12 (1,6%) patients under 18 years of age. Shigeyuki Ozaki [11] over 12 years from April 2007 to March 2019 operated >1100 patients. The mean age of the patients was 67,7±14,9 years. In general, the long-term survival rate within 12 years was 84,6%. Freedom from reoperation rate was 95,8%.
Study limitations. The main limitation of this study was the lack of medium- and long-term outcomes. We plan to monitor patients to obtain long-term results.
Conclusion
The Ozaki procedure is feasible and reproducible, has good short-term outcomes with excellent hemodynamic parameters. Further research is needed to assess long-term results.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Chernov I.I., Enginoev S.T., Komarov R.N., Bazylev V.V., Tarasov D.G., Kadyraliev K.B., Tungusov D.S., Arutyunyan A.V., Chragyan A.V., Batrakov P.A., Ismailbaev A.M., Tlisov B.M., Weymann А., Pompeu M., Zhigalov K. Short-term outcomes of Ozaki procedure: a multicenter study. Russian Journal of Cardiology. 2020;25:4157. https://doi.org/10.15829/1560-4071-2020-4157
Copy