Remote monitoring of outpatients discharged from the emergency cardiac care department
Аннотация
The coronavirus disease 2019 (COVID-19) pandemic has shown the need for the development of telemedicine technologies, especially remote follow-up using vital sign telemonitoring. In the Russian Federation, this approach is also justified by the remoteness factor with a shortage of medical workers in distant areas of the country.
Aim. To study the potential of remote monitoring in outpatients discharged after acute decompensated heart failure and acute coronary syndrome.
Material and methods. The study included 392 patients randomized to active follow-up groups with remote blood pressure (BP) monitoring (group 1, n=197) and standard management (group 2, n=195). The follow-up period lasted 3 months.
Results. During the follow-up period, patients managed with BP and heart rate telemonitoring tended to decrease in systolic BP from 132 (interquartile range (IQR), 121-139) mm Hg up to 125 (IQR, 115-130) mm Hg (p=ns). On the contrary, the 2nd group patients had a slight increase in systolic BP from 127 (IQR, 115-137) mm Hg up to 132 (IQR, 124-142) mm Hg (p=ns).
The patients of group 2 were more likely to receive diuretics and nitrates after 3-month follow-up, which can be considered a negative factor. This may indicate no improvement in the course of heart failure and chronic coronary artery disease with the absence of therapy correction over time.
During follow-up, four patients from group 1 were hospitalized due to decompensated heart failure or an episode of acute coronary syndrome with a total duration of 30 days, compared with 13 hospitalizations for the same reasons in group 2 (p=0,027; OR 3,4; 95% CI 1,1-10,8). In total, six patients died during the follow-up period in group 1, and eleven patients died in group 2 (p=0,226; OR 1,9; 95% CI 0,7-5,3). At the same time, three patients in the 1st group and one patient from the 2nd group died during the follow-up period due to COVID-19. Thus, cardiovascular mortality consisted of 3 and 10 patients in groups 1 and 2, respectively (p=0,052; OR 3,5; 95% CI 0,9-12,9).
Conclusion. Three-month remote management of patients after decompensated heart failure or acute coronary syndrome, including BP monitoring, showed a significant reduction in the hospitalization rate and a trend towards a decrease in cardiovascular mortality.
The most important hemodynamic factor that determines the prognosis for a number of cardiovascular diseases (CVD) is the level of blood pressure (BP). Arterial hypertension (AH) is the considerable modifiable risk factor for the development of cardiovascular complications and death [1][2]. At the same time, a negative effect of low BP on cardiovascular risk has also been found [3]. It has been shown that patients with AH have a J-dependent curve of blood pressure and cardiovascular outcomes [4].
Chronic heart failure (HF) remains a leading cause of disability and mortality with a high prevalence in the general population (7%). In the Russian Federation (RF), the average annual mortality is 6% in patients with functional class (FC) I-IV of HF, and 12% in patients with a pronounced clinical picture [5]. The increase in the prevalence of HF in the RF by 22% (from 6,7% to 8,2%) is of great concern, and that is clearly illustrated by the data of the recently completed EPOCH-CHF study [6].
The main reason of the formation of HF is acute and chronic forms of coronary artery disease (CAD). Obviously, an unfavorable prognosis in patients with HF is due to both the increase and the decrease in blood pressure, as well as the various forms of atrial and ventricular arrhythmias.
The pandemic of a new coronavirus infection has shown the unmet need for the development of telemedicine technologies, especially remote medical observation using telemonitoring of vital body functions. In the RF, this approach is also justified by the distance factor, when there is often a lack of medical workers in remote areas of our country.
The forecast of experts came true, who believed that mobile data traffic in Eastern Europe and Russia would have had six-fold increase by 2021 [7]. It is believed that more than 50% of patients going to the hospitals use the Internet resources to obtain data on their health status [8]. The significance of using telemedicine and its conceptual postulates are reflected in the official positions of international and major regional organizations (WHO, ESC, ACC/ AHA) [9-11]. Taking into account the fact that CVD is diagnosed in more than half of the population in developed countries, and 46-57% of deaths are associated with them, and the cost of management of patients with this pathology is >70% of the healthcare budget, it can be assumed that telemedicine along with standard approaches can significantly affect CVD statistics [12].
Objective: to study the potential of remote monitoring in outpatients discharged after acute decompensated heart failure and acute coronary syndrome.
Material and methods
The open randomized prospective study was performed on the basis of two research centers of the third level (university hospitals). A total of 392 patients were included in the study. Group 1 comprised patients (n=197, mean age of 66,3 [ 59,7- 73,5] years), incl. 94 women (49,3%) and 103 men (50,7%), who were actively controlled by remote BP monitoring (RBPM) using the oscillometric method. Monitoring was carried out with the certified INME01 tonometer (LLC INME, Russia) with an integrated GSM module that allows BP and pulse rate measurement, and the ability to transmit the results via a cellular communication channel to a research center. Based on the results of the received data, the doctor could contact the patient and adjust the previously prescribed treatment. In order to obtain a more informative BP value, the patient was recommended to perform at least three measurements with an interval of at least 1 min on the dominant upper limb. An additional measurement was recommended whether a difference in blood pressure was more than 5 mm Hg. Thus, the recommended number of measurements per session was three, which were performed at least twice a day in the morning (from 6,00 to 12,00) and in the evening (from 18,00 to 24,00).
Patients of group 2 (n=195, mean age of 66,2 [ 61,0-74,0] years), incl. 95 women (49,5%) and 100 men (50,5%), were recommended to carry out selfmonitoring of blood pressure, and drug treatment was adjusted by the district doctor. The duration of observation was 3 months.
Inclusion criteria for patients in the study:
1. Age over 18 years for both sexes.
2. Signed informed consent to participate in the study and consent to the processing of personal data.
3. Hospitalization for myocardial infarction (unstable angina) or acute decompensated HF, in the presence of HF symptoms equivalent to FC II-IV or ejection fraction <40%.
4. The ability to independently perform measurements of remotely controlled indicators.
The informing procedure was carried out with face-to-face contact between the researcher and the patient, following which the latter signed a written consent.
Exclusion criteria for patients in the study:
1. Possible alternative diseases that can mimic the symptoms of HF in a patient, such as:
- Chronic lung disease
- Primary pulmonary hypertension
- Chronic obstructive pulmonary disease with degree III-IV of bronchial obstruction.
2. Malignancy, other diseases/disorders or lifethreatening conditions that may prevent the participant to complete the study.
3. Alcohol and drug abuse, serious mental disorder.
4. Lack of technical ability to transmit measurement results (living outside the zone of stable coverage of the cellular network, etc.).
5. Pregnancy and lactation period.
6. Patient life expectancy <3 months.
7. Patient’s refusal to sign written informed consent to participate in the study.
Patients in the RBPM group received 4 visits. At visit 1, the patients were included in the study, informed consent was signed, and an individual registration card was filled out. Subsequently, medical telepatronage was carried out in the form of two visits performed in the mode of telemedicine video consultations after 1 and 2 months from the time of enrolment into the study. Wherein, complaints and anamnesis were collected, drug intake was monitored, and, if necessary, the previously prescribed treatment was corrected. It should be noted that if systolic blood pressure (SBP), diastolic blood pressure (DBP) and pulse values beyond the reference values were detected during RBPM, the doctor had the opportunity to contact the patient to correct therapy even outside the control visits. Visit 4 was performed after 3 months as a full-time appointment, during which the patient’s clinical condition was assessed, and the effectiveness of therapy was monitored.
Patients in the BP self-monitoring group received 2 visits. At visit 1, the patients were included in the study, informed consent was signed, and an individual registration card was filled out. Further management was carried out by the district doctor as needed; the patient independently went to the hospital in case of deterioration. Within 3 months the patient independently controlled the level of his pressure and pulse rate with a home tonometer. Visit 2 was carried out 3 months later in the form of a telemedicine consultation, during which the patient’s clinical condition was assessed, and the effectiveness of therapy was monitored.
The study was conducted in accordance with the current version of the Helsinki Declaration, the provisions of the Russian National Standard GOST R52379-2005 on Good Clinical Practice of April 01, 2006, the Order 200n of the Russian Ministry of Healthcare of April 1, 2016 “On Approval of the Rules of Good Clinical Practice” and Good Clinical Practice (GCP) guidelines.
Statistical analysis was carried out using SPSS Statistics Version 26. The Kolmogorov-Smirnov test was used to determine the normality of the distribution. Normally distributed continuous variables were presented as the mean (M) ± standard deviation (?). Abnormally distributed continuous variables were given as the median and interquartile range. Analytical statistics were performed using Student’s t-test for quantitative data with a normal distribution or the Mann-Whitney/Kruskal-Wallis test for quantitative data with an abnormal distribution. Fisher’s exact test was used to compare frequency scores between groups. Spearman’s method was used to analyze the relationship between the studied parameters. The significance level for testing hypotheses was taken equal to 0,05.
Results
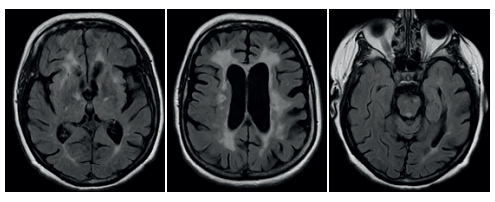
The nosological forms as the reasons for hospitalization in both groups are shown in Figure 1; more than 50% of those were acute and chronic forms of coronary artery disease.
Basically, both groups were comparable in age, gender, left ventricular ejection fraction, FC of HF, six-minute walk test distance, body mass index, SBP and DBP and heart rate (HR), the presence of comorbidities such as atrial fibrillation and flutter, diabetes mellitus, chronic kidney disease (Table 1, Figure 2).
During the follow-up period, there was a trend towards a decrease in SBP from 132 (interquartile range (IQR) 121-139) 125 (IQR 115-130) mm Hg (p=ns) in patients managed with BP and pulse telemonitoring. On the contrary, there was a slight increase in SBP from 127 (IQR 115-137) to 132 (IQR 124-142) mm Hg (p=ns) in group 2.
Evaluation of adherence to treatment in groups (Table 2) showed that group 1 had the best adherence for all groups of antihypertensive drugs, antiplatelet agents, anticoagulants and statins. However, there was a more frequent intake of diuretics and nitrates in group 2 during 3 months of follow-up. It could be regarded as a negative factor, since this may indicate the absence of positive dynamics in the course of HF and chronic coronary artery disease due to the absence of dynamic correction of treatment.
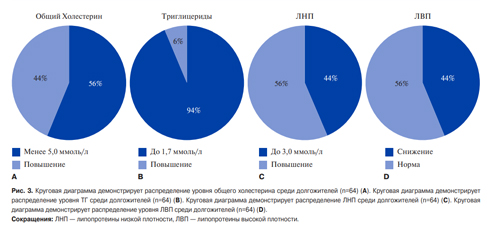
During follow-up, 4 patients from group 1 were hospitalized for HF decompensation or an episode of acute coronary syndrome with a total duration of 30 days, compared with 13 hospitalizations for the same reasons in group 2 (p=0,027; odds ratio (OR) =3,4; 95% confidence interval (CI) 1,1-10,8) with a total duration of 133 days (p=0,014). The distribution of hospitalized patients in the observation groups according to the diagnoses during the study is shown in Figure 3.

Figure 1. Quantitative and percentage ratio of nosological forms that caused the hospitalization in patients. A) in group 1; B) in group 2.

Figure 2. The number of patients with different FC of HF in the studied groups.
Abbreviation: FC — functional class.
Table 1
The main baseline and final parameters in the studied groups

Note: BMI1 — BMI at visit 1 in groups 1 and 2; BMI4/2 — BMI at visits 4 and 2 in groups 1 and 2, respectively; SBP1 and DBP1 — SBP and DBP at visit 1 in groups 1 and 2; SBP4/2 — SBP at visits 4 and 2 in groups 1 and 2, respectively; DBP4/2 — DBP at visits 4 and 2 in groups 1 and 2, respectively; Pulse1 — pulse rate at visit 1 in groups 1 and 2; Pulse4/2 — pulse rate at visits 4 and 2 in groups 1 and 2, respectively.
Abbreviations: DBP — diastolic blood pressure, BMI — body mass index, SBP — systolic blood pressure, DM — diabetes mellitus, 6MXT — 6-minute walk test, AF — atrial flutter, EF — ejection fraction, AF — atrial fibrillation, CKD — chronic kidney disease.
Table 2
Adherence to treatment in the studied groups

Note: * — р<0,05.
Abbreviation: ACE — angiotensin-converting enzyme.

Figure 3. The reasons for hospitalization during the observation period. A) in group 1; B) in group 2.
In total, 6 patients died during the follow-up period in group 1, and 11 patients died in group 2 (p=0,226; OR =1,9; 95% CI 0,7-5,3). At the same time, 3 patients in group 1 and one patient in group 2 died during the observation period from a new coronavirus infection. Thus, cardiovascular mortality was 3 people in group 1 (I25.1 — 2, I70.2 — 1) and 10 people in group 2 (G93.4 — 1, I25.1 — 3, I25.8 — 5, I21.1 — 1), р=0,052; OR =3,5; 95% CI 0,9-12,9.
In group 1, the analysis was also made of patients’ adherence to a new method of BP and heart rate controlling with telemedicine technologies. A total of 34741 BP measurements were performed by patients with the RBPM technique, measurements were taken over a period of 10843 days. Thus, the average number of measurements was of 3,2 per day. The number of measurements was of 13102 in the first month, 10985 in the second month (decrease by 18,7% in relation to the first month) and 10654 measurements in the third month of observation (decrease by 3% in relation to the second month). The same trend continued for the number of days on which measurements were made — 4049, 3442 (15% decrease) and 3352 (2,6% decrease) for each month of observation, respectively. The decrease in the total number of measurements could be due to a number of reasons: the death of several patients, their hospitalization, and also, to some extent, the loss of interest in the study. Meanwhile, the average number of measurements per day practically did not change during the follow-up and amounted to 3,24, 3,19, and 3,18, respectively, for 1, 2, and 3 months of follow-up, which was in line with the initial recommendations. The mean number of measurements per patient in group 1 was 176 (IQR 27-248); min 0, max 913; the average number of days of measurements was 55 (IQR 9-88); min 0, max 106.
During the observation period, 8569 (24,32%) episodes of high BP ?140 and 90 mm Hg were registered in the main group. Herewith, there was a tendency to reduce the number of such episodes during the study: 3850 cases were identified for the first month, 2449 ones were registered for the second month, and 1934 cases were revealed for the third month. The ratio of episodes of high BP to the total number of measurements for 1, 2 and 3 months of observation was 29,38%, 22,29% and 18,15%, respectively. The total number of episodes of hypotension (SBP ?90 mm Hg) was 658 measurements during the study period. Wherein, there was a trend towards a decrease in the number of such episodes during 1, 2 and 3 months, and that was 259, 204 and 197, respectively.
Episodes of tachycardia (HR ?100 bpm) and bradycardia (HR ?40 bpm) were also assessed. Tachycardia was noted in 963 cases during the entire observation period. In total, 403, 266, 293 episodes were registered for 1, 2 and 3 months of observation, respectively The overall number of episodes of bradycardia was 687 during the follow-up period, with a trend towards a decrease in the number of episodes of a rare pulse for 1, 2, and 3 months, and that was 255, 234 and 196 cases, respectively.
Discussion
Our data are comparable to a number of studies on the use of telemedicine technologies in the provision of medical care to patients with CVD. There was a higher probability of survival among patients in the intervention group compared with the control group after 1 year (adjusted relative risk (RR): 1,47, 95% CI 1,21-1,80, p<0,001) and 2 years (adjusted RR: 1,51, 95% CI 1,28-1,77, p<0,001), respectively. The authors made a fair conclusion that the probability of survival after 1 and 2 years was significantly higher in the active intervention group using telemedicine technologies [13].
A systematic review with direct meta-analysis of aggregated data using random effects models showed [14] that there was no difference in all-cause mortality between telemonitoring and conventional care. However, complex telemonitoring, which includes the transfer of patient data and analysis by specialists, reduces mortality from all causes (RR: 0,78, 95% CI 0,62-0,99; a total of 2885 people were analyzed in 12 randomized clinical trials (RCTs)). Evidence suggests that telemonitoring prevents HF-related hospitalizations (RR: 0,74; 95% CI 0,62-0,88; a total of 4001 people were included in 11 RCTs), structured telephone support reduces all-cause mortality (RR: 0,86; 95% CI 0,77-0,97; a total 9535 people in 24 RCTs) and HF-related hospitalizations (RR: 0,83; 95% CI 0,73-0,94; 7030 people were analyzed in 16 RCTs). The use of a mobile personal digital assistant prevents HF-related hospitalizations (RR: 0,58; 95% CI 0,44-0,77; a total of 674 people were included in 3 RCTs). The authors emphasize that clinicians should offer non-invasive monitoring using communication technologies to all patients with HF.
The long-term TEMA-HF study assessed whether an initial six-month telemonitoring program compared with conventional treatment would result in a reduction in all-cause mortality, hospitalizations for HF, and health care costs in long-term follow-up in patients with HF. The authors showed that this program led to a reduction in the number of days lost due to rehospitalization with heart failure [15].
A study based on comparing the effectiveness of office and home monitoring of 997 patients with HF using telemedicine technologies showed a 2-fold decrease in the number of hospitalizations in the group of patients with remote BP and ECG monitoring [16].
In Federal State Budgetary Institution “Almazov National Medical Research Centre” of the Ministry of Healthcare of the RF an analysis was made of the effectiveness of achieving targeted blood pressure and patient-oriented endpoints using telemonitoring in patients with hypertension. After 3 months, a significant decrease in “office” SBP and DBP was recorded in the telemonitoring group compared to the control group (p=0,002). By the end of the follow-up, BP parameters in the telemonitoring group decreased from 142±17 to 128±12 mm Hg (SBP), and from 88±8 to 79±6 mm Hg (DAD). Thus, a decline in SBP by -14±10 mm Hg (95% CI -11 to -17, r=0,819, p<0,0001) and DBP by -9±6 mm Hg (95% CI -7 to -11, r=0,647, p<0,0001) was achieved. There was also a decrease in the degree of anxiety and depression, according to Hospital Anxiety Depression Scale and the general condition of patients [17].
Federal State Budgetary Institution National Medical Research Center for Therapy and Preventive Medicine of the Ministry of Healthcare of the RF conducted an analysis of the economic feasibility of RBPM adoption using GPS-tonometers at the regional level by modeling. The authors showed that in a region of 1 million people RBPM would have prevented 1940 deaths over 5 years with 90% coverage of RBPM in patients with hypertension, and with 30% coverage, 645 lives could have been saved. The mass RBPM adoption will reduce the burden on the healthcare system by preventing myocardial infarctions (95 cases with 90% monitoring coverage over 5 years), strokes (630 with 90% coverage over 5 years) and ambulance calls. RBPM is economically feasible, because the cost of its implementation is less than the expected economic effect due to the reduction in requests for medical care and the preservation of labor resources in the economy [18].
Federal State Budgetary Institution National Medical Research Center for Therapy and Preventive Medicine of the Ministry of Healthcare of the RF together with Federal State Budgetary Institution National Medical Research Centre of Cardiology of the Ministry of Health of the RF carried out a study that made it possible to evaluate the clinical effectiveness of various telemonitoring models in monitoring BP in patients with hypertension. The study included 225 patients divided depending on the method of observation into 4 groups: the RBPM group in a round-the-clock mode with automatic transmission of measurement results (50 patients); the RBPM group during doctor’s working hours with automatic transmission of measurement results (50 patients); the RBPM group during doctor’s working hours with manual transmission of measurement results (50 patients); and the group of self-control of blood pressure (75 patients). Initially, the groups did not differ by age and sex, BP values. Six-month follow-up revealed a decline in mean BP values in all observation groups. There were no significant differences in this parameter when comparing the groups with each other. A large number of refusals to continue observation until the completion of the study were noted in groups that used manual data entry [19].
Interesting data were obtained in patients with HF using a remote monitoring platform [20]. The authors determined the possibility of increasing the ability of patients to self-help and self-control using a remote monitoring platform based on a mobile application in patients with HF. The authors based the remote monitoring platform on the Russian version of the European scale for assessing the ability of patients to self-care, which includes 9 points related to self-control issues. A lower score reflects a better ability of patients with HF to self-care. The followup period was 6 months. After 6 months, the average score on the scale in the mobile application group decreased to 15±2,3. While in the control group the average score was 23,95±3,02, which indicates a significantly better ability to self-care in the group of patients using the mobile application (p<0,001).
In our opinion, the effectiveness of telemonitoring in outpatients with HF for its decompensation or acute coronary syndrome is due to a number of reasons, among which are of particular importance: the territorial separateness in our country, the lack of medical workers in some medical organizations and remote areas, low adherence to the treatment in patients with chronic non-communicable diseases causing HF, a progressive course of circulatory failure requiring regular dynamic monitoring of vital body functions.
Conclusion
Three-month remote management of patients after decompensated heart failure or acute coronary syndrome, including BP monitoring, showed a significant reduction in the hospitalization rate and the trend towards the decrease in cardiovascular mortality.
Relationships and Activities: none.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Garanin A.A., Mullova I.S., Shkaeva O.V., Duplyakova P.D., Duplyakov D.V. Remote monitoring of outpatients discharged from the emergency cardiac care department. Russian Journal of Cardiology. 2022;27(3S):5072. https://doi.org/10.15829/1560-4071-2022-5072
Copy