Diastolic stress test in the preoperative non-cardiac surgery examination
Preoperative diagnostic tests in patients with chronic cardiovascular diseases before noncardiac surgery remain the discussion topic among surgery, therapy, and anesthesia professionals. Preoperative medical assessment of a patient undergoing high- risk elective noncardiac surgery requires identifying factors associated with both the type of surgery and comorbidity profile of each patient. Determination of clinically significant abnormalities of echocardio- graphic parameters, even without pronounced symptoms, can contribute to a change in management tactics or revision of timing and extent of surgery [1]. Transthoracic echocardiography (TTE) is an affordable diagnostic technique that is often used before major elective surgery in high-risk patients. However, defining echocardiographic criteria for potential postoperative cardiovascular complications, especially in asymptomatic patients with preserved left ventricular ejection fraction (LVEF) is an important clinical problem [2]. Diastolic stress test (DST) is currently an additional diagnostic tool to detect heart failure (HF) with preserved ejection fraction (HFpEF) in patients with LVEF >50% and even without symptoms in rest [3]. We will discuss the rationale for resting TTE and DST in surgical patients in this article.
Stratification of perioperative cardiovascular risk is a difficult task since almost half of all complications are observed in patients who were not initially considered a high-risk group or even without the previously diagnosed cardiac disease [4]. Modern guidelines for cardiovascular risk assessment in surgical patients are traditionally based on ruling out active or progressive changes in myocardial and intracardiac structures, assessing the risk of the operation itself, a patient>s functional status, and the presence of concomitant risk factors [5]. In European and US guidelines, TTE is considered as the main diagnostic method in high- risk patients [5][6]. The specificity of TTE in patients prior to elective noncardiac surgery is that it is not a standard screening method for evaluating all parameters. This is a targeted test aimed at identifying potential echocardiographic markers of a possible risk of complications during major surgery associated with endotracheal anesthesia, activation of the sympathoadrenal system, active intravenous transfusion therapy in case of blood loss, systemic inflammatory response syndrome, etc. Therefore, echocardiography in high- risk patients before noncardiac surgery should reflect the hemodynamic parameters as detailed as possible, especially in previously unexamined patients, older age patients, and those with comorbidities. Current guidelines involve preoperative TTE in the following categories of elective surgical patients:
- with shortness of breath of unclear origin or recent worsening of HF symptoms, or progressive decrease in exercise tolerance;
- for evaluating the heart valves in patients with different murmurs;
- in patients after open, minimally invasive and endovascular cardiac interventions [5][6].
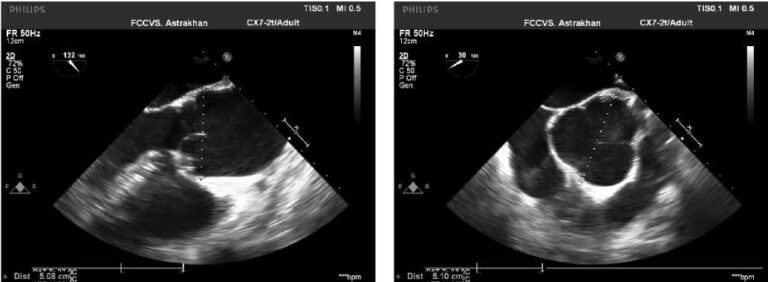
Echocardiography is also recommended for assessing the risk of perioperative complications in individuals with an initial moderate and high risk of cardiovascular perioperative complications in high-risk surgery [7]. TTE can provide complete information about myocardial dysfunction, valvular heart disease, myocardial contractility and hemodynamic disorders [8]. However, there is limited evidence regarding the benefits of routine preoperative echocardiography to assess preoperative risk. Some studies have suggested that data from TTE has no additional prognostic value. One population cohort study indicated that preoperative echocardiography and related data were not associated in any way with improving survival [7][9]. Some studies have shown that specific preoperative parameters of echocardiography can serve as markers of postoperative complications [10-12]. At the same time, there are data from a number of studies in which no significant relationship was found between LVEF and postoperative outcomes [13]. It has now been proven that individuals with preserved LVEF should not be considered as patients with a low risk of perioperative complications, since the risk of postoperative decompensated HF, major adverse events, arises at any LVEF, including values >50% [14]. This is probably why it was noted that patients with HFpEF and diastolic dysfunction are more prone to hemodynamic instability during surgery [15]. Filling pressure changes in patients with diastolic dysfunction may result from positive-pressure ventilation, decreased venous return, and impaired atrial contractility [16]. There is evidence of different effects of anesthetics on LV diastolic function [17]. Therefore, a detailed assessment of diastolic filling parameters is an important and necessary aspect of preoperative TTE. Symptoms associated with HF may not always be confirmed by resting echocardiography. In an elderly patient with multiple comorbidities with/without structural and/or functional impairment at rest, HFpEF is not always can be rule out. In patients with LV structural changes (increased LV mass index and/or left atrium (LA) volume index), but with normal resting filling pressure (E/e’<14), a stress test is recommended to assess LV diastolic filling during DST [18]. It also allows differential diagnosis of exertional dyspnea in patients with heart disease and noncardiac causes of dyspnea. Impaired relaxation is one of the earliest manifestations of LV diastolic dysfunction [2]. Relaxation properties gradually decrease with aging, obesity, diabetes, and hypertension. Most people with relaxation disorders do not have symptoms or signs of HF at rest [19]. However, exertional dyspnea and poor exercise tolerance are common in these patients, and therefore impaired LV relaxation is often a latent precursor to HF [20]. The diagnosis of an increase in the diastolic filling pressure in this group of patients is a difficult task and is based on identifying an increase in these parameters using ergometric testing [21]. A validated method for assessing LV filling pressure during exercise is cardiac catheterization [22]. This technique has an obvious limitation due to the technical complexity, but several studies have shown a good correlation between echocardiography, the ratio of early diastolic transmitral velocity (E) to early diastolic mitral annulus velocity (e’) and invasively measured LV filling pressure, both at rest and during exercise. Moreover, there is growing evidence that diastolic stress echocardiography provides important diagnostic data that can be useful in the management of asymptomatic patients and those with dyspnea of unclear origin [23]. Due to the increasing number of studies on validation of hemodynamic parameters and their prognostic value, the guidelines have provided recommendations for diastolic stress echocardiography [24]. In patients with unchanged diastolic function, LV filling increases during exercise without a significant increase in pressure. In healthy people with normal myocardial relaxation, it has been shown that E and e’ increase proportionally during exercise, which leads to a constant ratio of LV filling pressure — E/e’ [25][26]. During exercise in healthy people, LV untwisting increases and early diastolic filling maintains or increases stroke volume. In patients with HFpEF, LV filling decreases due to impaired early diastolic relaxation, and poor LV compliance leads to an inadequate increase in stroke volume during exercise, which leads to LV filling pressure increase. In patients with diastolic dysfunction, the e’, which reflects the myocardial relaxation, decreases at rest and does not increase during exercise to the same extent as in normal people, while the E increases due to increased LV filling in rest [27]. Many patients with HFpEF have symptoms, mainly during exercise, due to an increase in LV filling pressure. Exercise echocardiography provides a complete assessment of LV diastolic function. It was shown that the additional assessment of E/e’ with DST significantly improved the diagnostic accuracy of HFpEF detection [28][29][30]. The criterion for a positive DST is an induced increase in E/e’ >14. The test is usually carried out without medication withdrawal. If a patient use inhaled short-acting beta-agonists, it is not recommended to use them less than 3 hours before the stress test.
The first stage of DST consists of short resting echocardiography with assessing the following parameters:
- Е/e’,
- Pulmonary artery systolic pressure (PASP), mm Hg,
- LA end systolic volume index, ml/m2,
- LVEF (%).
The second stage is supine bicycle exercise test. The study is carried out with monitoring of hemodynamic parameters: blood pressure, heart rate (HR). The exercise period began with the subject riding 60 rpm at 50 W (<75 years of age) and 25 W (>75 years of age) and increasing the workload at 25 W each 3 min. When the HR reaches 100 bpm, the exercise continues for 3 minutes without increasing the workload. Further, during the test and/or within 5 minutes after stopping, the threshold values are estimated:
- E/e’ (threshold >14),
- PASP, mm Hg, (threshold >50),
- LA end systolic volume index, ml/m2 (threshold >34),
- LVEF (%) (no data on the threshold).
The criterion for stopping the test is the fully completed load within 3 minutes after reaching a HR of 100 bpm with the stable condition of a patient. There are following criteria for early stopping of the test: refusal to continue testing by a patient, increase in systolic blood pressure >220 mm Hg, the development of symptomatic arrhythmia, lower extremity pain, shortness of breath, which does not allow the study to continue. Echocardiography with DST also has limitations. It was shown that E/e’ was not measurable in about 10% of subjects; approximately 20% of the tests were considered false positive. But in case of controversial resting data, it is recommended to carry out hemodynamic DST, especially if the clinical decision depends on its result [31].
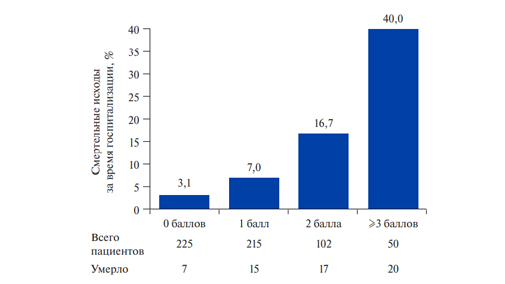
The relationship between abnormal increases in E/e’ during exercise and unfavorable outcomes is of clinical importance. The study by Holland DJ, et al. included 522 patients who underwent echocardiography with DST [32]. With a mean follow- up period of 13,2 months, patients with an isolated increase in E/e’ during exercise and isolated ischemia symptoms had a similar prognosis. An increase in E/e’ is a strong predictor of all-cause mortality, regardless of ischemia, age, and history of exertional dyspnea.
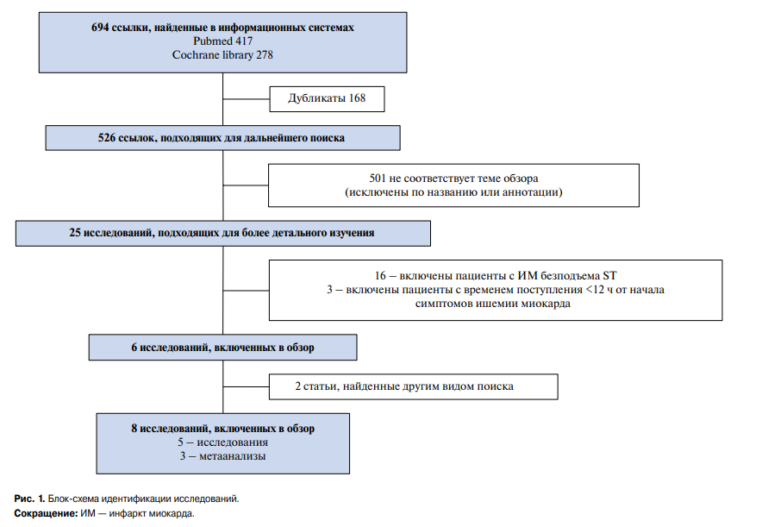
Verification of diastolic dysfunction in patients prior to noncardiac surgery is important. Thus, the study by Toda H, et al. showed that diastolic dysfunction is a predictor of perioperative myocardial injury [12]. The study by Cabrera Schulmeyer MC, et al. revealed that tissue Doppler-derived index E/e’ can be a useful predictor of complications after noncardiac surgery. In addition, it has been noted that patients with elevated preoperative E/e’ may require additional postoperative treatment [33]. Noninva- sive stress testing is now widely used for noncardiac surgery. Based on current clinical practice guidelines, physicians can use noninvasive stress testing in patients scheduled for a high-risk intervention or with a reduced or unclear functional status [34]. The rationale of the stress test for assessing ischemic disorders is a subject of discussion. Routine stress testing can lead to further unnecessary measures, including additional medical treatment, costly invasive procedures that may delay the elective surgery, or possibly increase the incidence of perioperative adverse events [34]. The largest meta-analysis on stress testing prior to noncardiac surgery was conducted, which left more questions than answers about its rationale. First, out of 40 studies, 36 were conducted without a comparison group, which indicates a low methodological quality. Second, in this meta-analysis, there was no significant difference in the risk of 30-day postoperative mortality associated with a positive/negative preoperative stress. Third, out of 1807 studies reviewed, 485 (26,8%) were excluded because they did not measure severe outcomes such as mortality, myocardial infarction, or heart failure. Thus, the available data are insufficient to conclude whether stress testing improves the assessment of perioperative risk [35]. All of these studies examined the stress-induced myocardial ischemia. There are currently no data on the use of DST for assessing perioperative risk before noncardiac surgery. It is promising and important to continue research in this direction, which will include not only patients with coronary artery disease, but also other categories of cardiac patients.
Conclusion
Experience with DST in HFpEF patients considers the potential benefit of this method prior to noncardiac surgery for more accurate cardiovascular risk stratification. The introduction of simple exercise measurements will provide additional relevant diagnostic information. The fact that noninvasive DST can also be performed with any type of ergometer machines opens up even more prospects for wide clinical use. Of particular value for patients prior to noncardiac surgery is that DST is of clinical importance in patients with dyspnea of unclear origin and in asymptomatic patients with comorbidities. Therefore, further observational studies are needed to assess the predictive value of DST in patients prior to noncardiac surgery.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Dzhioeva O.N., Drapkina O.M. Diastolic stress test in the preoperative non-cardiac surgery examination. Russian Journal of Cardiology. 2020;25(3S):3986. https://doi.org/10.15829/1560-4071-2020-3986
Copy