Conservative therapy for external myocardial rupture in a patient with anterior myocardial infarction: a case report
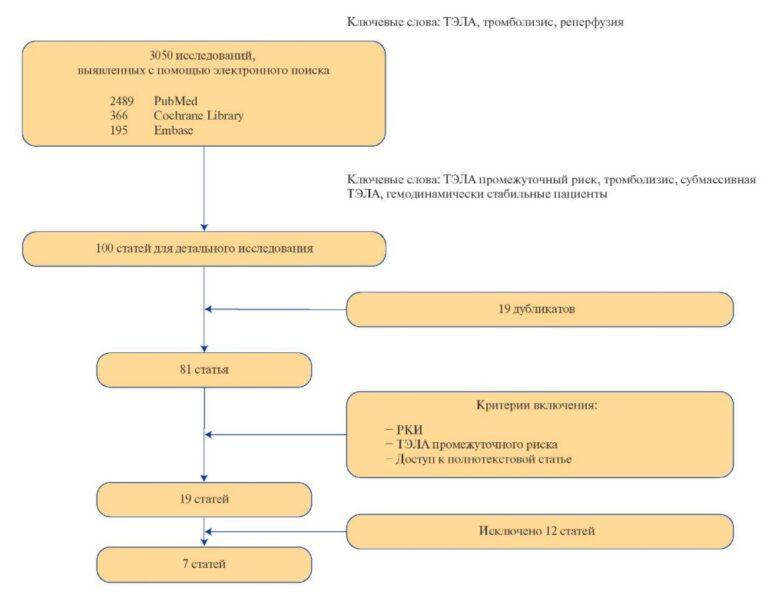
Myocardial rupture is one of the most severe complications of myocardial infarction (MI), which accounted for up to 30% of in-hospital mortality in prereperfusion era. The large-scale development and implementation of reperfusion therapy has significantly improved the outcomes of patients with myocardial infarction, dramatically reducing mortality and the incidence of mechanical complications in MI. Studies of the last 35 years have identified such important risk factors for myocardial rupture as primary myocardial infarction, anterior and lateral MI, large necrotic area, female sex, age (over 70 years), persistent ST segment elevation, stable hypertension, recurrent angina, late seeking medical help, unsuccessful reperfusion in young patients [1][2].
As an example, we would like to present the following case report: 56-year-old female patient with hypertension for about 15 years (increased blood pressure (BP) up to 180/100 mm Hg), who occasionally took antihypertensive drugs. Previously, she tolerated exercise satisfactorily. The patient became ill on April 26, 2020, when suddenly felt retrosternal pressing pain radiating to the left subscapularis, lasting ~1 hour, accompanied by cold sweat. Prehospital electrocardiography (ECG) revealed ST segment elevation in V2-V6, I, AVL leads by 4 mm, heart rate of 96 bpm (Figure 1). The pain syndrome was prehospitally arrested with morphine, and thrombolytic therapy (streptokinase) was also carried out within 30 minutes. The patient was admitted to the Department of Urgent Cardiology of the M. Mirrakhimov National Center of Cardiology and Internal Medicine 1,5 hours after the pain onset with a following diagnosis: ST segment elevation acute coronary syndrome. Killip class IV.

Figure 1. The patient’s Initial ECG.
The patient was admitted in an extremely serious condition with signs of cardiogenic shock (BP of 60/40 mm Hg, cold sweat, paleness). The infusion of inotropic agents was immediately started (dopamine 5-10 ?g/kg/min with BP monitoring), as well as antiplatelet agents were given (clopidogrel 300 mg, aspirin 250 mg). Due to absence of reperfusion according to ECG, 1,5 hours after the thrombolytic therapy (Figure 2), the patient underwent percutaneous coronary intervention.

Figure 2. The patient’s ECG 1,5 h after thrombolysis.
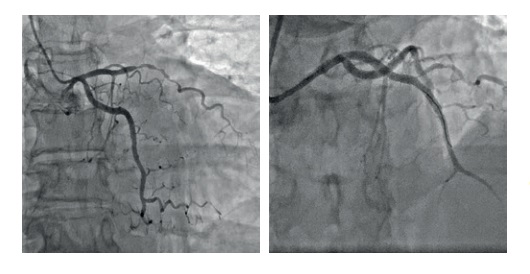
Coronary angiography showed the following abnormalities: right dominant coronary circulation, class 2 occlusion in the middle third of anterior descending artery (immediately after the first diagonal branch leaves), TIMI 0, 75% stenosis at diagonal branch orifice; irregular circumflex branch contour, TIMI III, 75% stenosis in the middle third of right coronary artery, TIMI III. Drug-eluting stenting were placed in 6-7 segments of anterior descending artery. Further coronary angiography showed patent anterior descending artery without signs of thrombosis and dissection, TIMI III (Figure 3).

Figure 3. Coronary angiography before and after stenting of the anterior descending artery
Despite the measures taken, the patient’s condition remained severe. Against the background of cardiogenic shock, there were signs of acute renal injury (glomerular filtration rate of 17 ml/min/1,73 m2), acute encephalopathy. Transthoracic echocardiography (Table 1) revealed akinesia of the middle and apical segments of interventricular septum, the anterior and lateral left ventricular (LV) walls, as well as diastolic separation of pericardial layers by 1,2 cm behind the posterior and lateral LV walls, at the apex — 0,8 cm due to external myocardial rupture. The entire pericardial cavity is filled with fibrin deposits of moderate echogenicity.
An additional echo signal (parietal thrombus) of 2,7×1,6 cm was located in the apex from LV side, under which an echo-free space of 1,6×0,9 cm (myocardial rupture) was visualized (Figure 4, 5). Blood flow through the myocardial rupture site was not determined.

Figure 4. Transthoracic echocardiography of the patient.
Note: apical 2-chamber view: diastolic separation of pericardial layers — 1,2 cm behind the LV posterior and lateral walls, at the apex — 0,8 cm due to external myocardial rupture; below, there is an echo-free space of 1,6×0,9 cm (myocardial rupture site).
Abbreviation: LV — left ventricle.

Figure 5. Transthoracic echocardiography of the patient.
Note: LV parasternal short axis view: pericardial cavity is filled with fibrin deposits of moderate echogenicity. An additional echo signal (parietal thrombus) is located in LV apex area.
Abbreviation: LV — left ventricle.
The patient was examined by a cardiac surgeon, who recommended emergency surgery, which she refused. Conservative therapy was continued in the form of dopamine infusion at a rate of 5-10 ?g/ kg/min with BP monitoring, diuresis stimulation (intravenous furosemide at a dose of 20-60 mg a day with water balance and glomerular filtration rate monitoring), anticoagulant therapy (heparin), statins, taking double antiplatelet therapy. By the 4th day of hospitalization, the patient hemodynamics stabilized: BP of 120/70-115/60 mm Hg was maintained without sympathomimetic therapy. To stabilize the condition, angiotensin-converting enzyme inhibitors and beta-blockers were prescribed. By the time of discharge, the patient had decreased levels of transferases (aspartate aminotransferase — 25,6 U/L, alanine aminotransferase — 35,2 U/L). Glomerular filtration rate was also improved — 52 ml/min/1,73 m2. The patient was able to walk 20 meters.
Repeat echocardiography showed improved LV contractility (Table 1) — LV ejection fraction increased to 34%. Akinesia of interventricular septal middle and apical segments, anterior and lateral LV walls persisted due to LV aneurysm development. Diastolic separation of pericardial layers was 0,9 cm behind the posterior and lateral LV walls, at the apex — 0,6 cm.
Table 1
Echocardiographic characteristics of the patient

Abbreviations: LV — left ventricle, RV — right ventricle.
The patient was discharged on the 14th day. After discharge, the patient was recommended to take two antiplatelet agents, an angiotensin-converting enzyme inhibitor, a diuretic, a statin, a beta-blocker, and spironolactone. In the future, it was planned to carry out surgical treatment.
Re-examination was carried out 9 months after MI. According to echocardiography, there was a further improvement in LV contractility (Table 1) — LV ejection fraction has reached 43%. There was akinesia and bulging of interventricular septal middle and apical segments, apical segments of LV anterior, lateral and inferior walls. In other areas, hyperkinesia was determined. Pericardial layers were compacted and thickened due to hemopericardum remodeling. Behind the LV posterior wall, adhesive process was revealed. An insignificant echo-free space was determined along the LV lateral wall (Figure 6). The patient had steady state and compensated at NYHA class IIII heart failure. She is adherent to all recommendations for secondary prevention. She still categorically refuses surgery.

Figure 6. Transthoracic echocardiography of the patient.
Note: apical 2-chamber view: pericardial layers are compacted and thickened due to hemopericardium remodeling; behind the LV posterior wall, adhesive process is visualized.
Abbreviation: LV — left ventricle.
Discussion
The most informative methods for diagnosing myocardial rupture include left ventriculography, transthoracic echocardiography [3]; computed tomography [4]. In our case, the most accessible method for diagnosing myocardial rupture was echocardiography, according to which the rupture itself and hemopericardium was detected.
Treatment of myocardial rupture consists of emergency surgery. Currently, there are many approaches to the surgical treatment of myocardial rupture [5]. However, sometimes, for various reasons, it is not possible to carry out surgery. The described case is interesting for several reasons. The patient was admitted in an extremely serious condition, with MI complicated by myocardial rupture and cardiogenic shock. There were serious limitations in the choice of drug and treatment methods. Streptokinase, clopidogrel, and dopamine were used, while there was no intra-aortic balloon counterpulsation, not to mention other options for mechanical circulation support. Despite this, it was possible to perform coronary artery stenting and stabilize the patient’s condition. Along with therapeutic interventions, a certain role in the outcome was specified by chance circumstance, namely, the location of LV thrombus over rupture site, and later the closure of defect by adhesions. Currently, the patient has stabilized at NYHA class IIII heart failure and carefully follows the recommendations for secondary prevention. Echocardiography shows an improvement in LV contractility. Considering that myocardial revascularization was successfully performed, no surgical treatment is currently planned. In the near future, taking into account the patient’s wishes, contrast-enhanced coronary computed tomography angiography will be performed and then the additional treatment will be planned.
Чтобы читать статью войдите с логином и паролем от scardio.ru
Keywords
For citation
Beishenkulov M.T., Chazymova Z.M., Kaliev K.R., Toktosunova A.K., Madyarova Y.M., Dadabaev M.Kh. Conservative therapy for external myocardial rupture in a patient with anterior myocardial infarction: a case report. Russian Journal of Cardiology. 2021;26(2S):4289. https://doi.org/10.15829/1560-4071-2021-4289
Copy